礼来公司在新墨西哥州开始对COVID-19中和抗体bamlanivimab(LY-CoV555)进行研究
2020-12-19 Allan MedSci原创
礼来公司今天宣布,通过与新墨西哥州的当地机构合作,已开始对COVID-19中和抗体bamlanivimab(LY-CoV555)进行研究。
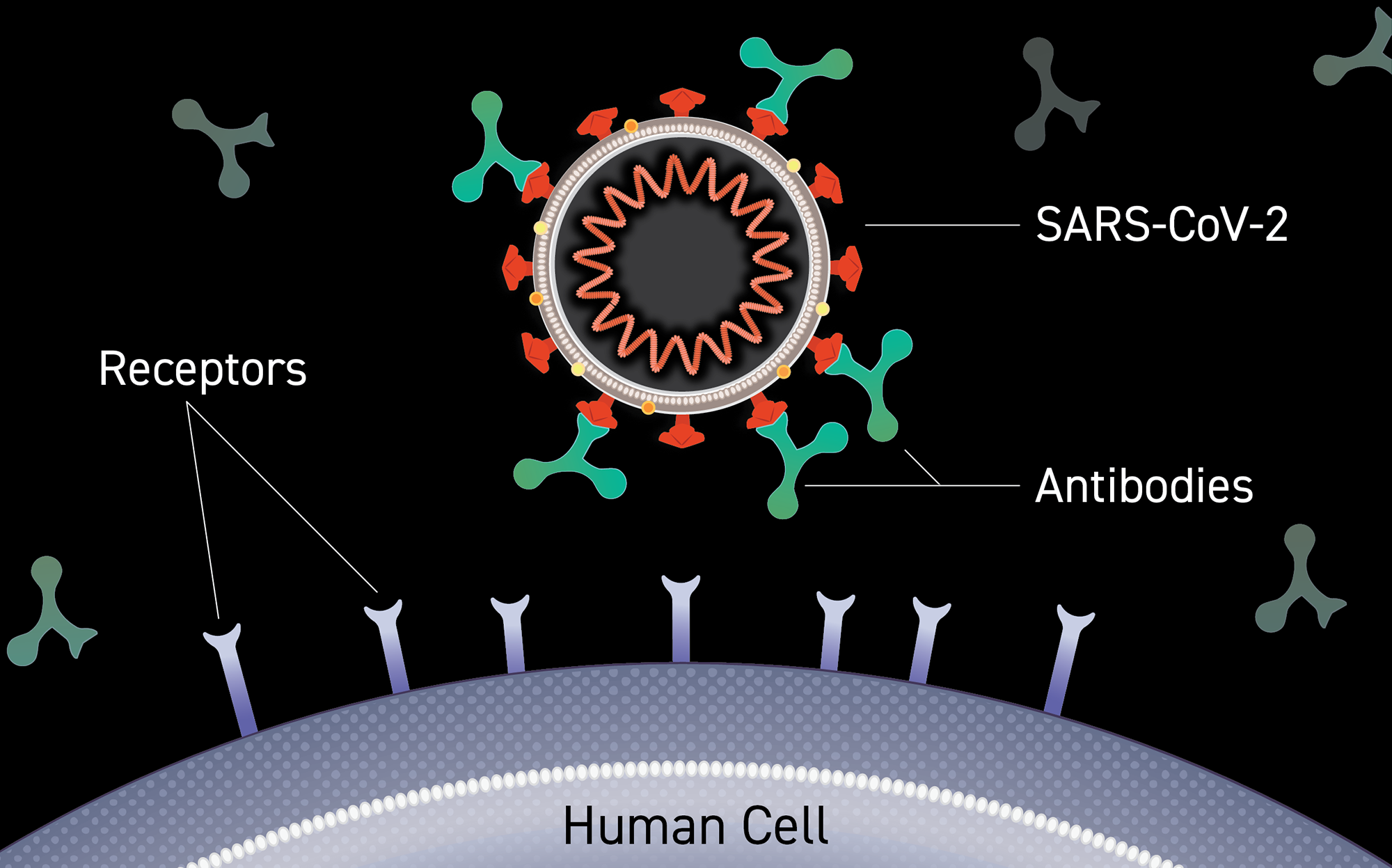
礼来公司今天宣布,通过与新墨西哥州的当地机构合作,已开始对COVID-19中和抗体bamlanivimab(LY-CoV555)进行研究。在新墨西哥州进行的研究将允许在现实世界中收集bamlanivimab的有效性和安全性的数据。
Bamlanivimab最近获得了美国食品药品监督管理局(FDA)的紧急使用授权(EUA),用于治疗轻度至中度COVID-19患者和/或COVID-19住院患者。

礼来公司首席科学官Daniel Skovronsky博士说:“建立bamlanivimab的证据基础是非常重要的。除了收集疗效和安全性数据外,礼来公司还将利用这项研究来探索在各种环境中使用bamlanivimab的情况,这可能有助于指导最佳实践”。
这项研究将在未来几周内开始,并将评估bamlanivimab在减少高危人群中COVID-19住院方面的有效性。根据研究设计,新墨西哥州将使用各种输液技术,从而使不同社区的患者能够使用bamlanivimab,包括美洲印第安人社区。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#墨西哥#
30
#mAb#
22
#NIV#
30
#IVIM#
0