APOLLO研究:Aumolertinib在中国获批用于EGFR T790M阳性NSCLC患者
2021-11-26 小文子 MedSci原创
aumolertinib是一种有效且耐受性良好的第三代EGFR TKI。
Aumolertinib(阿美替尼,原名 almonertinib;HS-10296)是一种新型三代表皮生长因子受体(EGFR)酪氨酸激酶抑制剂(TKI),可选择性抑制EGFR致敏和 T790M突变。Journal of Thoracic Oncology杂志发表文章报告了APOLLO研究的最新成果。APOLLO是在中国进行的评估aumolertinib治疗EGFR T790M突变晚期NSCLC的疗效和安全性的研究。
研究纳入经一代或二代EGFR TKI治疗后发生EGFR T790M突变阳性的局部晚期或转移性非小细胞肺癌(NSCLC)患者244例。患者在禁食状态下(给药前1小时/给药后2小时不进食)口服110 mg Aumolertinib,每日一次,连续21天循环,直到疾病进展、出现毒性反应或患者退出等。主要终点客观缓解率(ORR)。
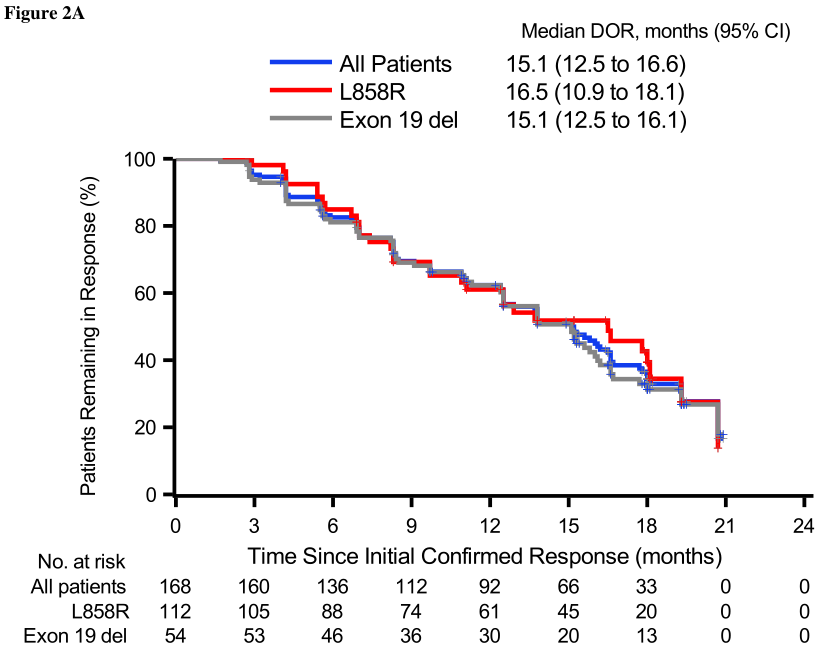
中位随访时间19.4个月(IQR: 13.3-20.8),中位缓解时间6.1周(95% CI: NR-NR),ORR为68.9%(168/244,95% CI:62.6%-74.6%)。疾病控制率(DCR)为93.4%(228/244,95% CI:89.6%-96.2%)。EGFR外显子19缺失和L858R突变患者的中位缓解持续时间(DOR)分别为15.1个月(95%CI:12.5-16.1)和16.5个月(95%CI:10.9-19.3)。中位无进展生存期(PFS)为12.4个月(95% CI:9.7-15.0)。
在 23例可评估的中枢神经系统(CNS)转移患者中,IC-ORR 和IC-DCR 分别为60.9%(95% CI:38.5-80.3)和91.3%(95% CI:72.0-98.9)。中位IC-DOR 为12.5个月(95% CI:5.6-NR)。
40例(16.4%)患者发生≥ 3级治疗相关不良事件,最常见的是血肌酸磷酸激酶升高(17/244,7%)和丙氨酸转氨酶升高(3/244,1.2%)。244例患者的aumolertinib平均剂量密度为109.0 mg,每日一次,代表相对剂量密度为99.2%。
结果表明,aumolertinib是一种有效且耐受性良好的第三代EGFR TKI,在中国获批用于第一代和第二代EGFR TKI治疗后疾病进展的EGFR T790M阳性NSCLC患者。
原文出处:
Lu S, Wang Q, Zhang G, et al, Efficacy of Aumolertinib (HS-10296) in Patients with Advanced EGFR T790M+ NSCLC: Updated Post NMPA-approval Results from the APOLLO Registrational Trial, Journal of Thoracic Oncology (2021), doi:https://doi.org/10.1016/j.jtho.2021.10.024.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#SCLC患者#
23
#阳性NSCLC#
54
#T790M#
23
不错
51
#NSCLC患者#
24
#GFR#
19