J Thorac Oncol:综合分析TP53和KEAP1突变在非小细胞肺癌(NSCLC)中的预后价值
2021-10-03 yd2015 MedSci原创
TP53和KEAP1突变是局部期NSCLC(I-IIIA期)患者的预后因素,而KEAP1突变是晚期(IIIB-IV期)患者的预后因素。
TP53和KEAP1突变在非小细胞肺癌(NSCLC)中比较常见,但它们的预后价值尚不明确,特别是在局限性肿瘤中。近期,来自德国的团队开展了真实世界回顾性研究,评估TP53和KEAP1突变在非小细胞肺癌(NSCLC)的预后价值。相关结果发表在Journal of Thoracic Oncology杂志上。
这是在德国进行的多中心真实世界的回顾性队列研究。局部期(UICC分期I-IIIA)患者和晚期(UICC分期)患者IIIB-IV)患者分别进行分析。主要研究终点是总生存期(OS)。
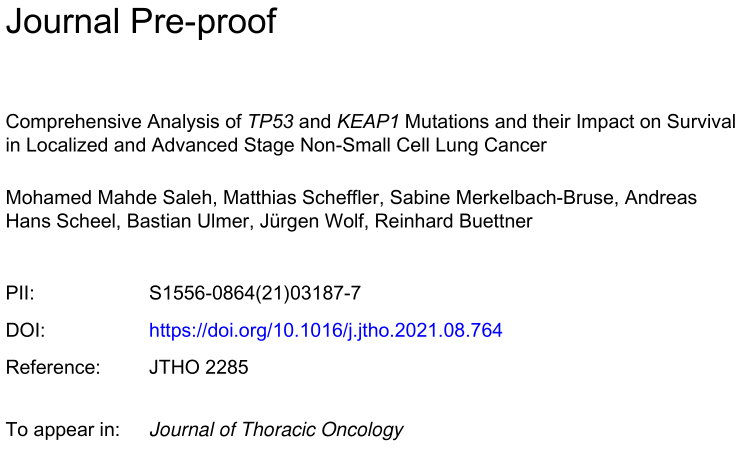
对6297例NSCLC患者的OS进行了分析。中位随访时间为642天。超过一半的肿瘤(3245/6297,51.5%)伴有TP53突变,1 /6(524/3022,17.3%)伴有KEAP1突变。对于TP53,大多数突变是错义突变(2334),其次是截断突变(640)、内框突变(57)和其他突变,包括同义词和未编码突变(214)。错义突变聚集在已知热点,最常见的密码子为157、158、179、245,248、249和273。对于KEAP1,发现了类似的突变分布:大多数是错义突变(380),其次是截断突变(97)和其他突变(20)。
两者突变分布
对于局部期患者(I-IIIA期),大多数为男性(60.1%),腺癌(70.4%)。半数以上的患者(50.6%)无淋巴结受累。T4有13.8%,T2有37.7%。大部分患者首次诊断为UICC IIIA期(42.5%),其次为I期(29.8%)和II期(27.7%)。临床相关突变分布如下:8.9%为EGFR突变,1.5%为BRAF V600E突变,1.8%为ALK/ROS易位,28.5%为KRAS突变,17.0%为KEAP1突变,5.5%为NFE2L2突变。
TP53突变与男性、鳞状组织、EGFR、KRAS和ALK/ROS的野生型状态以及NFE2L2突变显著相关。截断TP53突变与鳞状上皮组织学、首次诊断时较高的UICC分期和KRAS的野生型状态显著相关。KEAP1突变与男性和EGFR和NFE2L2的野生型状态显著相关。
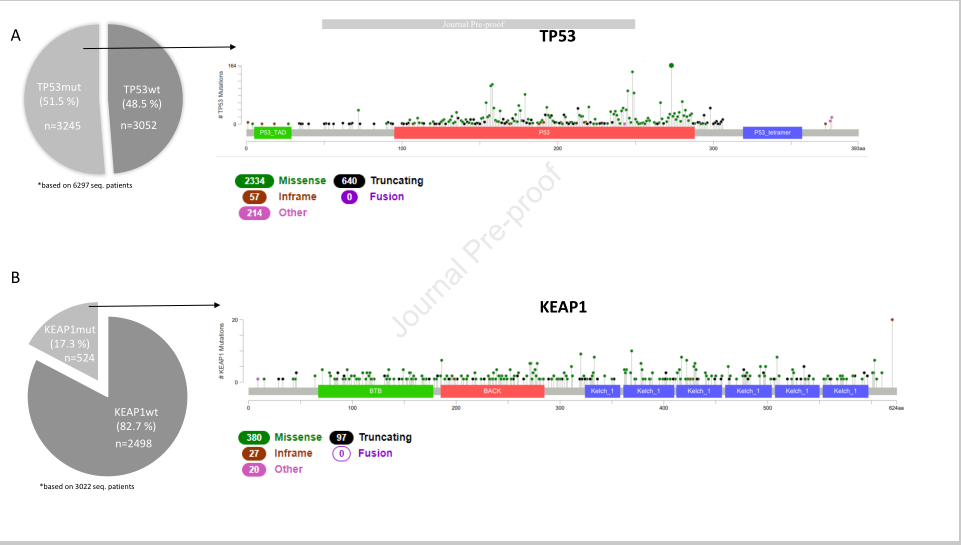
TP53截断突变患者的中位OS为1181天(95% CI, 818 to 1543),而TP53野生型患者的为1474天 (95% CI 1232 to 1751),TP53其他突变的为1486天 (95% CI, 1133 to 1838) (HR =1.61 [95% CI 1.22 to 2.12]; P=0.001)。此外,无论突变类型如何,与TP53野生(TP53wt)肿瘤相比,TP53突变患者的无病生存期(DFS)显著缩短(TP53wt为791天,TP53其他突变为630天,TP53截断突变为657天)。
局部期突变对OS影响
KEAP1突变(KEAP1mut)组患者的中位OS为755天(95% CI 500 - 1010),而KEAP1野生(KEAP1wt)组的中位OS为1264天(95% CI 1116 - 1412)(HR=1.74 [95% CI 1.3 - 2.33];p=0.001)。与TP53类似,KEAP1mut患者的DFS明显短于KEAP1wt患者(732天vs 473天)。
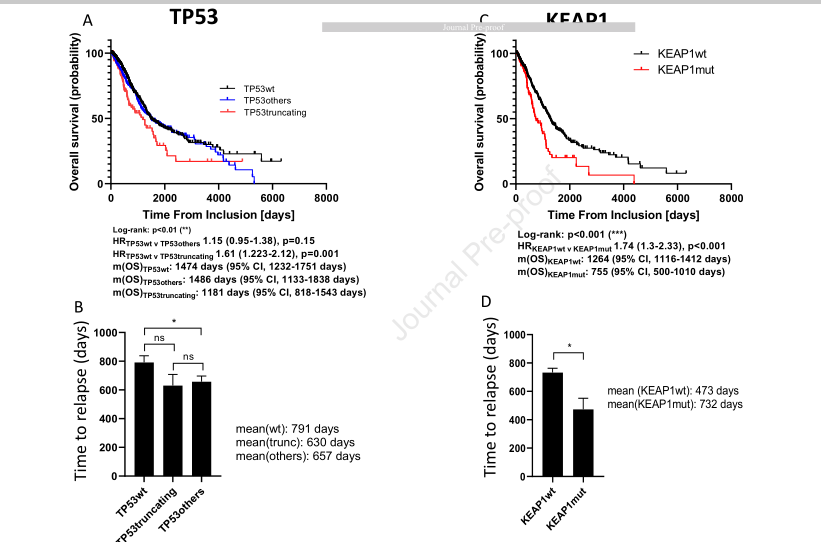
多因素分析,经过对相关因素调整后,TP53截断突变(HR=1.43 [95% CI 1.07 to 1.91] , P=0.015) 或KEAP1突变(HR=1.69 [95% CI 1.25 to 2.28], P=0.001)是影响患者的独立预后因素。
局部期OS多因素分析
对于晚期患者(UICC IIIB-IV),多为男性(56.2%),腺癌(81.5%)。近四分之三的患者有淋巴结转移(72.5%)。大多数晚期患者诊断为UICC IV期(81.5%)。临床相关突变分布如下:12.7%为EGFR突变,1.6%为BRAF V600E突变,3.2%为ALK/ROS易位,31.6%为KRAS突变,17.4%为KEAP1突变,3.4%为NFE2L2突变。
4818例晚期患者中50.9%存在TP53突变。TP53mut队列中的患者明显更有可能是男性,组织学呈鳞状,首次诊断时UICC分期较低,肿瘤大小较大,KEAP1、NFEL2和ALK/ROS处于野生型状态。TP53截断突变与KEAP1突变显著相关。KEAP1突变与较高的年龄、腺瘤组织学、男性、较大的肿瘤大小、EGFR、ALK/ROS、NFE2L2和TP53的野生状态显著相关。
TP53截断突变患者的中位OS为448天 (95% CI 375 to 520),而TP53野生型患者的为506天(95% CI 463 to 549),TP53其他突变的为436天(95% CI 392 to 480) (HR = 1.06 [95% CI 0.93 to 1.22], P=0.379)。
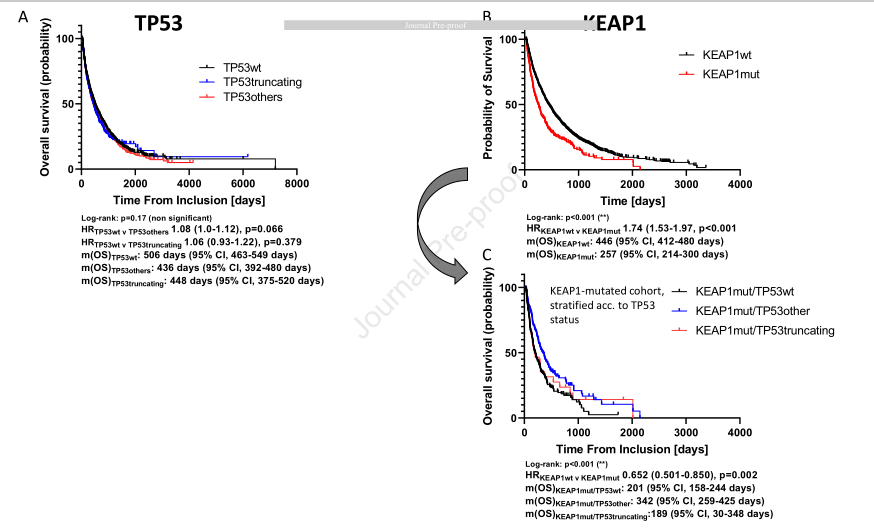
晚期患者突变对OS影响
KEAP1突变(KEAP1mut)组患者的中位OS为257天 (95% CI 214to 300),而KEAP1野生(KEAP1wt)组的中位OS为446天 (95% CI 412 to 480) (HR= 1.74 [95% CI 1.53 to 1.97], P<0.001)。与TP53类似,KEAP1mut患者的DFS明显短于KEAP1wt患者(732天vs 473天)。
KEAP1mut / TP53other组患者的中位OS为342天(95%CI 259 - 425),KEAP1mut / TP53wt组患者的中位OS为201天(95% CI 158 - 244),KEAP1/TP53截断突变组患者的中位OS为189天(95% CI 30 - 348) (HR=0.65(95%CI 0.50-0.85),P = 0.002)。
多因素分析,经过对相关因素调整后,KEAP1突变(HR= 1.40 [95% CI 1.27 to 1.61], P<0.001)是影响患者的独立预后因素。
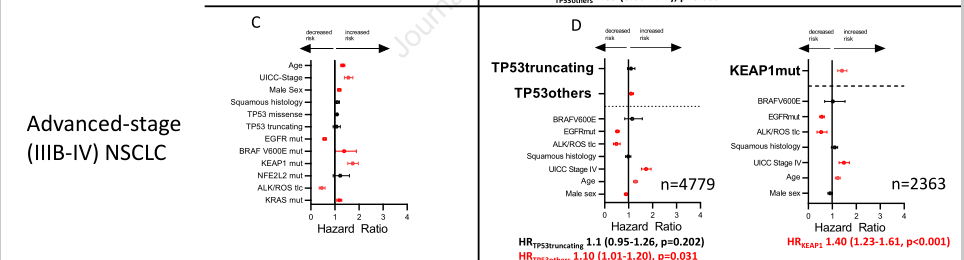
晚 期OS多因素分析
综上,TP53和KEAP1突变是局部期NSCLC(I-IIIA期)患者的预后因素,而KEAP1突变是晚期(IIIB-IV期)患者的预后因素。
原始出处:
Saleh MM, Scheffler M, Merkelbach-Bruse S, Scheel AH, Ulmer B, Wolf J,Buettner R, Comprehensive Analysis of TP53 and KEAP1 Mutations and their Impact on Survival in Localized and Advanced Stage Non-Small Cell Lung Cancer, Journal of Thoracic Oncology (2021), doi: https://doi.org/10.1016/j.jtho.2021.08.764.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#THORAC#
41
#非小细胞#
37
#Oncol#
51
#p53#
57
#预后价值#
50
#TP53#
89
#Keap1#
41
TP53的确不好
67
医学进步
61
好文章,谢谢分享。
71