J Periodontal Res:人老化牙龈成纤维细胞的炎症、增殖和细胞骨架反应改变
2020-02-13 lishiting MedSci原创
组织结构和功能降低是老化的特征,它可以理解为是由于细胞老化而产生。然而,对于获取老化牙龈成纤维细胞的表型反应的研究还较少。为此,这篇研究的目的是为了评估原代培养的人牙龈成纤维细胞增殖是否会影响与细胞老化以及组织衰退相关的细胞功能。
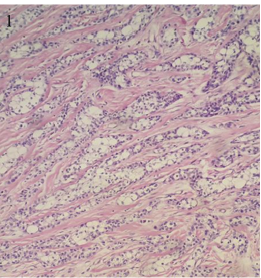
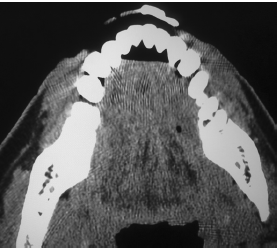
组织结构和功能降低是老化的特征,它可以理解为是由于细胞老化而产生。然而,对于获取老化牙龈成纤维细胞的表型反应的研究还较少。为此,这篇研究的目的是为了评估原代培养的人牙龈成纤维细胞增殖是否会影响与细胞老化以及组织衰退相关的细胞功能。研究从5位年轻供体中获取人的牙龈成纤维细胞并培养直至细胞老化。通过观察和分析细胞大小、细胞增殖、p16和p21 mRNA水平、H2Ax磷酸化、细胞活性以及老化相关的b-半乳糖苷酶染色评估细胞老化情况。通过分析细胞因子的分泌以及NF-κB的核转位评估炎症水平。通过胶原凝胶收缩测定检测胶原重塑。通过免疫荧光和激光共聚焦观察细胞骨架蛋白的定位。通过paired sample t检验或the Wilcoxon matched-pairs signed-rank检验分析实验数据以确定同一供体培养的早几代细胞和晚几代之间的变化。结果显示,晚几代的细胞变化与细胞老化相一致,包括细胞变大,细胞增殖降低,SA-beta gal染色阳性,磷酸化的H2Ax,以及p16和p21 mRNA表达水平增加。晚几代的细胞胶原收缩减少,并且细胞骨架蛋白actin和vinculin的共区域化降低
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
30
#牙龈成纤维细胞#
33
#成纤维细胞#
42
#老化#
40
#纤维细胞#
32