European Radiology:MRI在预测结直肠癌肝转移患者早期复发方面的价值
2022-08-25 shaosai MedSci原创
磁共振成像(MRI)是最有价值的无创工具,可用于病变检测和分类以及反应评估,并为根治性手术提供最准确的指示。
据统计,约有50%至60%的结直肠癌患者在病程中出现肝转移。对于最初可切除的结直肠癌肝转移灶(CRCLM)患者来说,完全切除肝转移灶是一种潜在的根治性治疗手段,可获得高达50%的5年和20%的10年生存率。遗憾的是,最初只有少数患者可以进行根治性切除。此外,高达60%的CRCLM患者在手术后出现早期复发,这表明这类CRCLM患者并不适合手术。
磁共振成像(MRI)是最有价值的无创工具,可用于病变检测和分类以及反应评估,并为根治性手术提供最准确的指示。除了肿瘤的大小和数量,MRI还可以为我们提供更多信息。已有人尝试根据MRI上肿瘤的延迟增强以及MRI扫描的纹理和放射组学特征来预测CRCLM患者术后的预后。然而,放射组学特征和筛查受到扫描仪类型、使用的扫描参数和重建算法的影响,这导致迫切需要对图像数据进行规范化和标准化。
多项研究发现,肿瘤边界具有预测肿瘤早期复发的潜力。有报道称CRCLM的组织病理学生长模式(HGPs)对总生存期有预示作用。然而,术前MRI上的肝转移瘤生长模式是否能预测接受治愈性手术的CRCLM患者的早期复发仍是未知数。
近日,发表在European Radiology杂志的一项研究探讨了CRCLM患者术前MRI上肝转移瘤的生长模式与术后早期复发之间的关系,并通过CRCLM的HGPs对最终结果进行判析,为临床快速、早期、无创的评估CRCLM患者的风险及预后提供了参考依据。
共有来自3个独立中心的348名CRCLM患者入组,包括初级队列中的130名339个肝转移患者和验证队列中的218名患者。参照肝细胞癌(HCC)的大体分类,将每个肝转移灶在MRI上的生长模式分为四种类型:粗糙型、平滑型、病灶外突型(FEP)和结节融合型(NC)。使用Kaplan-Meier方法构建无病生存(DFS)曲线。
在初级队列中,339个肝转移灶中42个(12.4%)是粗糙型,237个(69.9%)是光滑型,29个(8.6%)是FEP型,31个(9.1%)是NC型。那些有FEP-和/或NC型肝转移的患者比没有这种转移的患者DFS更短(P < 0.05)。然而,粗糙型和光滑型肝转移患者与无此类转移的患者之间的DFS没有明显差异。在两个外部验证队列中,有FEP-和/或NC型肝转移的患者的DFS也比没有这种转移患者的DFS短。此外,40.5%的高风险型(FEP和NC)肝转移瘤在新辅助化疗后转为低风险型(粗糙和光滑)。
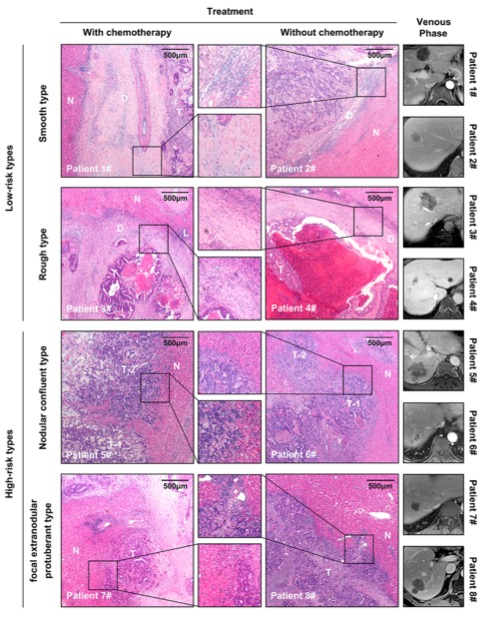
图 原发人群中不同生长模式的肝转移瘤病理表现。D,脱髓鞘的边缘;N,正常肝实质;L,淋巴细胞浸润;T,肿瘤组织
本研究结果表明,对肝转移瘤生长模式的评估可以增加术前常规MRI的临床价值,有利于术前对复发概率高的患者进行早期识别并制定最佳的治疗方案。
原文出处:
Qian Cai,Yize Mao,Siqi Dai,et al.The growth pattern of liver metastases on MRI predicts early recurrence in patients with colorectal cancer: a multicenter study.DOI:10.1007/s00330-022-08774-8
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#早期复发#
47
#PE#
55
#肝转移#
62
#结直肠#
50