Front Genet:原发性胆道胆管炎对甲状腺功能障碍的影响
2022-01-25 从医路漫漫 MedSci原创
原发性胆道胆管炎(PBC)是一种自身免疫性胆汁淤积性肝病,并伴有其他进行性加重的疾病。

背景:原发性胆道胆管炎(PBC)是一种自身免疫性胆汁淤积性肝病,并伴有其他进行性加重的疾病。其患病率和年发病率分别为每百万居民6.7至492例和0.7至49例。PBC可导致肝硬化、肝癌、肝衰竭,大多在10年内死亡。随着PBC的发病率和并发症的增加,其发病机制是值得我们进一步研究的。众所周知,高达73%的PBC患者有肝外表现(如干燥综合征、甲状腺功能障碍和系统性硬化症),其高发病率降低了生活质量。其中,甲状腺功能障碍在PBC患者中发生率为5.6%-23.6%,明显多于无PBC患者。甲状腺可以调节人体生长、神经元发育、生殖和能量代谢,甲状腺功能障碍是由甲状腺激素分泌过多或不足引起的,可能导致甲状腺功能减退等各种甲状腺疾病。有研究表明,部分患者同时存在甲状腺功能减退症状和PBC症状,PBC患者甲状腺功能减退的发生率增加。据报道,PBC患者的血清促甲状腺激素(TSH)水平和平均血清游离甲状腺素(FT4)水平较高。这两种激素失衡也出现在肝硬化患者中。此外,PBC是一种自身免疫性肝病(AILD),患者罹患其他自身免疫性疾病的风险更高,包括自身免疫性甲状腺疾病(AITD)、桥本甲状腺炎和Graves甲状腺炎。然而,上述PBC与甲状腺功能障碍之间的关系是基于观察性研究得出的,其中反向因果关系、选择偏倚,特别是未观察到的混杂因素可能会掩盖真正的因果关系。有必要进一步研究这些相关性背后的因果关系。
方法:我们使用两样本孟德尔随机化(MR)方法来评估PBC对欧洲人群中自身免疫性甲状腺疾病(AITD)、促甲状腺激素(TSH)和游离甲状腺素(FT4)、甲状腺功能亢进、甲状腺功能减退和甲状腺癌(TC)风险的潜在因果关系。共收集了7组PBC和相关性状的数据集,进行了一系列MR分析,并进行了广泛的敏感性分析,以确保结果的可靠性。
结果:通过敏感性分析,我们发现PBC是AITD、TSH、甲状腺功能减退和TC的危险因素,比值比(OR)为1.002 (95% CI: 1.000-1.005, p ?(95%置信区间:1.006-1.027,p ?0.002), 1.068 (95% CI: 1.022-1.115, p ?和1.106 (95% CI: 1.019-1.120, p ?分别为0.042)。有趣的是,使用反向MR分析,我们还发现AITD与PBC有显著的潜在因果关系,OR为0.021 (p ?5.10E−4),其他两者对PBC无显著因果关系。

图1 PBC对AITD的MR分析总结。(A) IV、MR- egger和IVW的MR效应量。(B) PBC对AITD因果影响的散点图。我们用垂直和水平的黑线分别表示静脉注射对PBC (x轴)和AITD (y轴)估计效果的95% CI。我们用红线表示IVW随机效应模型。(C) PBC对AITD因果关系的漏斗图。每个点表示每个IV的估计因果效应。垂直的深蓝色线表示使用MR-Egger方法得到的因果效应估计;浅蓝色的线表示使用IVW方法获得的因果效应估计。先生,孟德尔随机化;PBC:原发性胆管炎;AITD,自身免疫性甲状腺疾病;第四,工具变量;IVW,逆方差加权。

图2 PBC对TSH的MR分析总结。(A) IV、MR- egger和IVW的MR效应量。(B) PBC对TSH因果效应的散点图。我们用垂直和水平的黑线分别表示静脉注射对PBC (x轴)和TSH (y轴)估计影响的95% CI。我们用红线表示IVW随机效应模型。潜在的SNP异常值(rs11065987和rs2076310)用绿色高亮显示。(C) PBC对TSH因果关系的漏斗图。每个点表示每个IV的估计因果效应。垂直的深蓝色线表示使用MR-Egger方法得到的因果效应估计;浅蓝色的线表示使用IVW方法获得的因果效应估计。潜在的SNP异常值(rs11065987和rs2076310)用绿色高亮显示。先生,孟德尔随机化;PBC:原发性胆管炎;TSH,促甲状腺激素;第四,工具变量;IVW,逆方差加权;SNP(单核苷酸多态性。
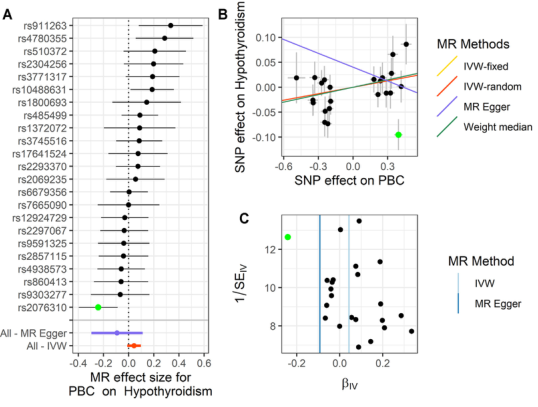
图3 甲状腺功能减退患者PBC的MR分析总结。(A) IV、MR- egger和IVW的MR效应量。(B) PBC对甲状腺功能减退因果关系的散点图。我们用垂直和水平的黑线分别表示静脉注射对PBC的估计影响的95% CI (x轴)和对甲状腺功能减退的95% CI (y轴)。我们用红线表示IVW随机效应模型。潜在的SNP异常值(rs2076310)用绿色高亮显示。(C) PBC对甲状腺功能减退因果关系漏斗图。每个点表示每个IV的估计因果效应。垂直的深蓝色线表示使用MR-Egger方法得到的因果效应估计;浅蓝色的线表示使用IVW方法获得的因果效应估计。潜在的异常值(rs2076310)用绿色高亮显示。先生,孟德尔随机化;PBC:原发性胆管炎;第四,工具变量;IVW,逆方差加权;SNP(单核苷酸多态性。
结论:PBC可引起甲状腺功能障碍,具体表现为AITD、轻度甲状腺功能减退、TC。PBC与甲状腺功能障碍的潜在因果关系为PBC的病因学研究提供了新的方向。
原文出处:Huang P, Hou Y, Zou Y,et al.The Causal Effects of Primary Biliary Cholangitis on Thyroid Dysfunction: A Two-Sample Mendelian Randomization Study.Front Genet 2021;12
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#NET#
47
#原发性#
48
#Gene#
56
#Genet#
46
#功能障碍#
42
#胆管#
50