Nat Chem Biol: 哈佛大学研究发现:一组分子有望治疗帕金森病
2020-06-18 Lauren 转化医学网
帕金森病是一种常见的神经功能障碍疾病,主要影响中老年人,是继肿瘤、心脑血管病之后中老年的“第三杀手”。
帕金森病是一种常见的神经功能障碍疾病,主要影响中老年人,是继肿瘤、心脑血管病之后中老年的“第三杀手”。帕金森的治疗多年来一直停滞不前。但近日,新加坡南洋理工大学(NTU Singapore)和哈佛大学(Harvard University)的一项研究发现,一对有前景的分子为开发一种缓解帕金森病的新疗法带来了希望。

近日,新加坡南洋理工大学(NTU Singapore)和哈佛大学(Harvard University)的一项研究发现,一对有前景的分子为开发一种缓解帕金森病的新疗法带来了希望。
帕金森病是仅次于阿尔茨海默症的第二大最常见的神经退行性疾病,影响全球700万至1000万人。帕金森病患者大脑中的多巴胺水平降低,导致他们难以控制自主运动,出现手部、手臂和腿部肌肉震颤和僵直等症状。他们也会出现一些非运动症状,例如睡眠障碍、抑郁和嗅觉丧失。
通过实验室调查和体内实验,来自南大生物科学学院的尹浩燮(Yoon Ho Sup)教授和来自美国金麦克莱恩医院和哈佛医学院的金光洙(Kwang-Soo Kim)教授领导的研究小组发现,一组“分子对”前列腺素E1(PGE1)(一种激素)和前列腺素A1(PGA1),是提高多巴胺水平和减缓帕金森病的关键。
PGE1和PGA1能够与Nurr1结合,Nurr1是一种对大脑多巴胺的发育和维持至关重要的蛋白质。
它们的结合会导致Nurr1被激活,会导致多巴胺大量产生,也能够防止产生多巴胺的脑细胞的死亡。在激活Nurr1之后,患有帕金森病的小鼠的运动功能有显着改善。
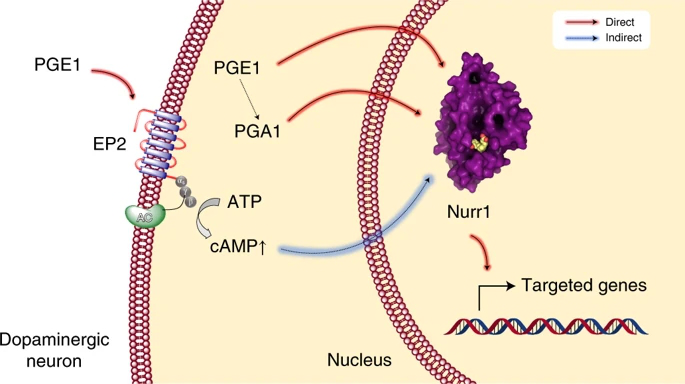
图解摘要
尽管仍有许多研究需要进行,但这些发现能够为开发激活Nurr1的药物来对抗帕金森病提供了新的途径。帕金森是目前无法治愈的疾病,虽然已经有了一些治疗方法,像生成多巴胺的药物治疗或使用电流进行深部脑刺激,但这些治疗方法都有副作用,只能解决病人的症状,不能缓解或抑制帕金森病。
尹教授表示,“考虑到nurr1的基本功能,我们一直在寻找它在体内的激活分子。最终,我们成功地识别出,PGE1和PGA1是针对Nurr1特异作用的分子对,可以对大脑产生神经保护作用。鉴于所有的候选帕金森药物都未能在临床试验中显示出神经保护的能力,我们的发现可能为设计基于机制的疾病改善疗法提供机会,以几乎没有任何副作用的方式治疗帕金森病。”
该研究在2020年5月发表在同行评审期刊《自然化学生物学》上,是由来自新加坡、美国和韩国的研究人员共同完成的。
前列腺素(PGE1/PGA1)——对抗帕金森病的关键
前列腺素是人体中一些类似激素的物质之一,负责广泛的身体功能,如平滑肌的收缩和松弛,血管的扩张和收缩,控制血压,调节炎症。
它们在激活Nurr1多巴胺功能中的调控作用目前尚未被研究。
为了识别和表征PGE1/PGA1激活Nurr1的方式,研究团队使用核磁共振和X射线晶体学来破译相关分子的结构,首次成功揭示了PGA1结合导致激活Nurr1的细节。
这些来自细胞实验的发现随后得到了实验诱发帕金森病的体内实验的支持,这些实验显示,当使用PGE1和PGA1时,它们的运动功能得到了显着改善。
金教授表示:“通过揭示分子间的相互作用,我们对Nurr1在健康和疾病(如帕金森病)中的生物学功能和调节有了深入的了解。我们在这项研究中的发现增加了我们对多巴胺神经元如何工作的了解,并指向帕金森病新疗法的发展。”
南大李光前医学院研究副院长、合着者林嘉梁(Lim Kah Leong)教授强调了这项发现的重要性,他说:“PGA1并不是新生分子,而是一种具有抗炎症和抗肿瘤特性的分子。前列腺素如PGE1可用于临床,例如产科病例。这意味着,这种化合物有可能被重新定位,用于治疗帕金森患者,从而加快将实验性药物送到临床所需的时间。”
目前,科学家们正在寻找一种合成形式的PGE1/PGA1,并验证它作为一种潜在的新药,可以针对Nurr1,从而阻止或逆转帕金森病的发病。
原始出处:Sreekanth Rajan, Yongwoo Jang, Chun-Hyung Kim, et al. PGE1 and PGA1 bind to Nurr1 and activate its transcriptional function. Nature Chemical Biology. 25 May 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#研究发现#
30
#Nat#
32
#Bio#
42
#哈佛#
32
#Biol#
33
#帕金森病#
156