Blood:应以微小残留病灶检测阴性作为高风险多发性骨髓瘤的治疗终点
2020-08-04 MedSci原创 MedSci原创
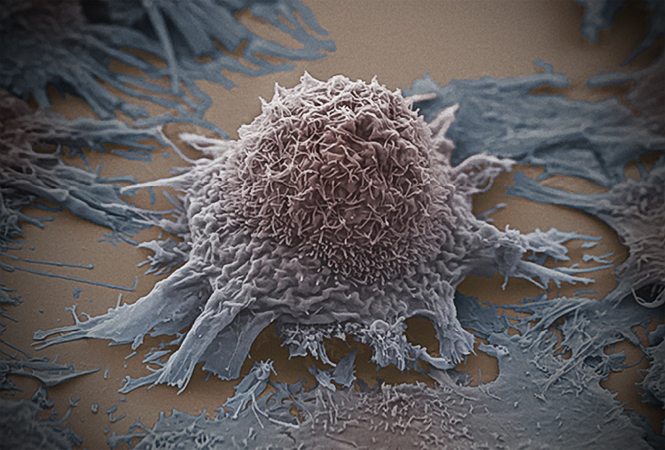
与标准细胞遗传学异常(CA)风险的病例相比,携带高CA风险的多发性骨髓瘤(MM)患者尽管达到了相似的完全缓解(CR)率,但预后较差。
与标准细胞遗传学异常(CA)风险的病例相比,携带高CA风险的多发性骨髓瘤(MM)患者尽管达到了相似的完全缓解(CR)率,但预后较差。这质疑了CR作为高危型MM的治疗终点的合理性,并且代表了对于标准和高危型CA患者在治疗后仍然残留肿瘤细胞的生物学难题。
Goicoechea等采用二代流式(NGF)来评估PETHEMA/GEM2012MENOS65试验招募的标准(n=300) vs 高 CA风险(n=200)的MM患者的可检测的残留病灶(MRD),以明确两个患者亚组中决定MRD抵抗的机制。
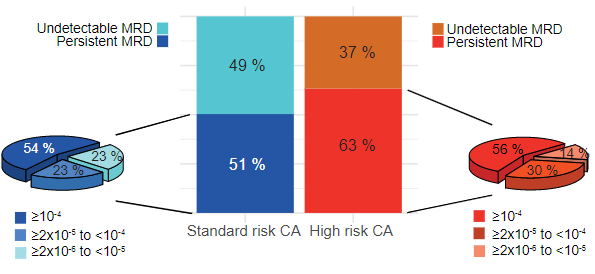
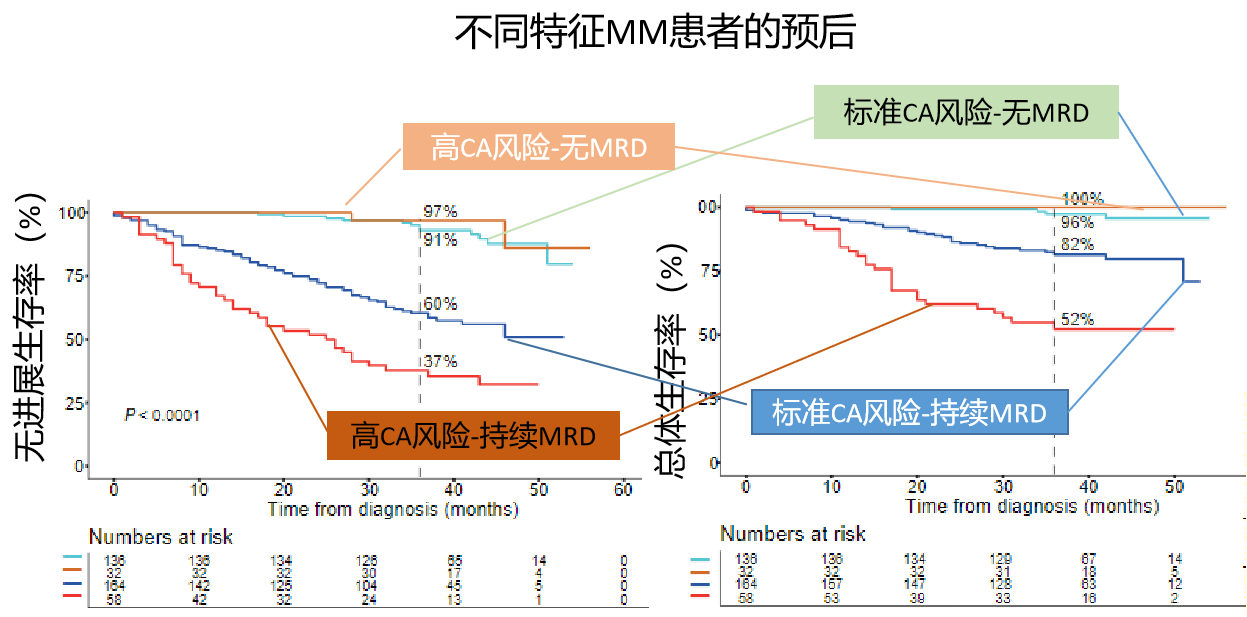
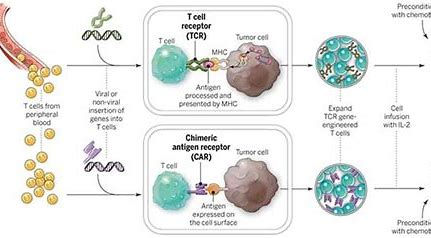
未检测到MRD的患者的36个月无进展生存期和总生存率均高于90%,具有标准风险或高 CA风险的病例之间无明显差异(P≥0.202)。持续MRD导致标准和高 CA风险患者的中位无进展生存期分别大约只有3年和2年(P<0.001)。
进一步用NGF分离MRD,然后对配对的MRD肿瘤细胞进行全基因组测序,发现具有标准CA风险的MM患者的克隆选择更多,高风险MM患者有更多的继发突变、基因组不稳定性更高,未发现驱动MRD抵抗的统一的缺失或获得性遗传变异。
相反,MRD肿瘤细胞的RNA测序揭示了高风险MM中具有单一转录程序和ROS介导的MRD抵抗的MRD克隆选择。本研究支持将无法检测到MRD作为高CA风险的MM患者的治疗终点,并提议表征MRD克隆以了解和克服MRD抵抗。
原始出处:
Ibai Goicoechea,et al. Deep MRD profiling defines outcome and unveils different modes of treatment resistance in standard and high risk myeloma. Blood. July 21,2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#高风险#
35
#多发性#
37
👌
86
#微小残留病灶#
38
学习
88