JAMA Otolaryngol Head Neck Surg:一种预测重度手术并发症的前庭神经鞘瘤临床分期系统
2021-10-26 AlexYang MedSci原创
建立一个肿瘤分期系统,通过结合发病时的症状和肿瘤的大小来预测严重的手术并发症情况。
根据丹麦的流行病学研究以及明尼苏达州奥姆斯特德县的一项基于人口的研究,在过去40年里,前庭神经鞘瘤(VS)的发病率一直在上升。这种情况可能的原因是医疗保健的普及及诊断技术的进步。当发现这些肿瘤时,考虑到肿瘤的生长速度缓慢与治疗有关的发病率,需要对治疗方案进行仔细的研究。采用手术治疗、放疗或主动监测受多因素的影响,包括年龄、合并症、初始肿瘤大小、生长速度、听力状况和病人的偏好。

长期以来,前庭神经鞘瘤一直作为一个同质实体来对待,其临床症状可能有助于阐明肿瘤亚型的基本病理生理学特征。描述这些良性肿瘤的异质性有助于预测治疗相关的临床结果。
近期,来自美国的研究人员在《JAMA Otolaryngol Head Neck Surg》上发表文章,他们建立一个肿瘤分期系统,通过结合发病时的症状和肿瘤的大小来预测严重的手术并发症情况。
研究纳入了1998年1月1日至2020年10月13日,在一个单一三级转诊中心的患者队列。研究的主要结果为手术后30天内出现的严重手术并发症,并由Clavien-Dindo分类系统确定。出现3级或以上并发症的患者确定为发生严重并发症。
研究结果发现,在评估的185名患者中,40名(22%)有严重的术后并发症。40名患者中有20名(50%)是女性;平均(SD)年龄为46(13)岁。出现严重并发症的患者具有较大肿瘤(最大直径>2.5厘米)、前庭症状,近期出现听力损失的可能性较高。研究人员结合临床症状和发病时的肿瘤大小,创建了一个4级临床严重程度分期系统,用来预测严重并发症。临床严重程度分期系统显示,新系统对严重并发症的鉴别能力(C指数,0.754;95%CI,0.67-0.84)比单纯的肿瘤大小模型(C指数,0.706;95%CI 0.62-0.79)更好。
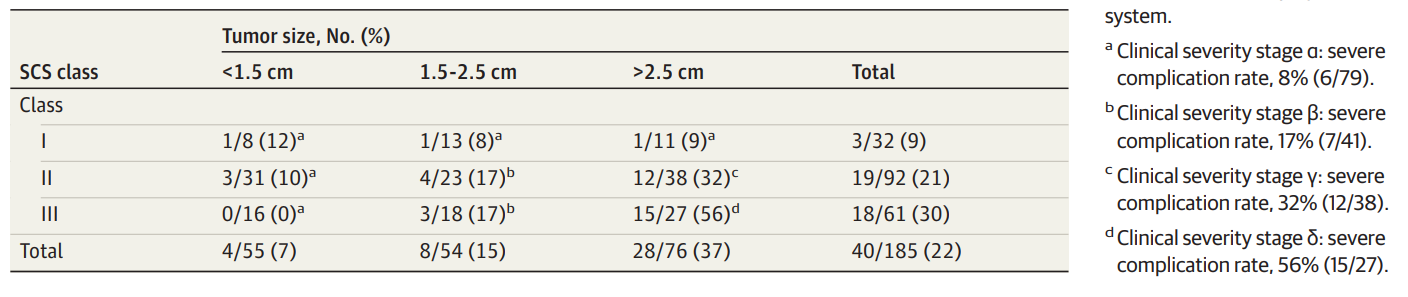
预测术后严重并发症的临床分期系统(结合了症状分类和肿瘤大小)
综上所述,前庭神经鞘瘤患者中,除肿瘤大小外,初次评估时出现的临床症状也可用于预测术后严重并发症。因此,他们建立的结合发病时症状的新临床严重程度分期系统,可以帮助临床医生识别术后出现严重并发症的高风险患者。
原始出处:
Harrison J Smith , Nedim Durakovic , Bhuvic Patel et al. Clinical Staging to Estimate the Probability of Severe Postoperative Complications in Patients With Vestibular Schwannoma. JAMA Otolaryngol Head Neck Surg. Oct 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#NEC#
43
#并发#
37
#神经鞘瘤#
63
#手术并发症#
41
#前庭神经#
46