Nat Commun:科学家发现胰腺癌的潜在治疗靶点
2022-04-21 生物谷 生物谷
研究发现USP25作为PDAC肿瘤生长和活力所需的基本DUB,可促进病理性 HIF-1驱动的代谢重编程,是胰腺癌的潜在治疗靶点。
胰腺导管腺癌(PDAC)是一种高度致死性疾病,5年生存率低于9%,预计到2030年将成为癌症死亡的第二大原因。PDAC肿瘤的侵袭性和对传统化疗的耐药性被认为是由于缺乏临床上可靶向的突变、免疫细胞耗尽的缺氧微环境、代谢的改变和肿瘤的异质性导致的。去泛素化酶(DUBs)在靶向蛋白降解中发挥着重要作用,代表着癌症的一种新兴治疗模式。然而,它们在胰腺导管腺癌(PDAC)中的治疗潜力还没有被探索出来。
近日,发表在Nature Communications上的一篇题为“USP25 promotes pathological HIF-1-driven metabolic reprogramming and is a potential therapeutic target in pancreatic cancer”的学术论文,发现USP25作为PDAC肿瘤生长和活力所需的基本DUB,可促进病理性 HIF-1驱动的代谢重编程,是胰腺癌的潜在治疗靶点。

在本研究中,为了鉴定PDAC中的酶活性DUB,研究人员开发了一种将泛素-ABPs与质谱法相结合的分析管道,将基于活性的蛋白质组学与患者衍生的PDAC类器官和小鼠遗传模型中的功能丧失遗传筛查相结合。通过PDAC类器官中的功能丧失遗传筛选测定了DUBs的功能意义,将USP25鉴定为PDAC肿瘤生长和活力所需的基本DUB。接下来,他们通过沉默Usp25在KPCY类器官中的表达来评估其生物学作用,发现USP25的耗竭导致患者来源的类器官活力,存活率降低和体内PDAC肿瘤生长减弱。因此,USP25在PDAC生长和维持中起着至关重要的作用。
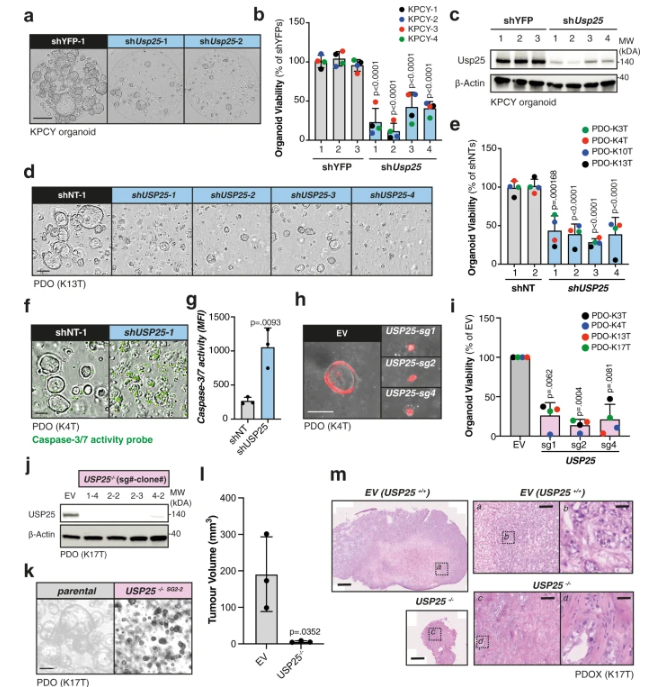
图 USP25的消耗导致患者来源的类器官形成,活力和体内PDAC肿瘤生长减弱
研究进一步发现,USP25通过调节缺氧诱导因子-1α(HIF-1α)的稳定性和转录活性是糖酵解的主调节剂。为了评估Usp25在PDAC中的作用,研究人员比较了它在PDAC中的表达和酶活性与健康胰腺组织中的表达和酶活性,结果发现,与正常胰腺组织相比,USP25在PDAC中具有高表达和酶活性,这与患者生存期较差相关。此外,遗传和药理学USP25抑制导致PDAC类器官的强效生长障碍,而正常的胰腺类器官不敏感,并导致患者来源的异种移植物急剧消退。从机制上讲,USP25可去泛素化并稳定HIF-1α转录因子。PDAC的特征在于严重缺氧的微环境,USP25消耗会使HIF-1α转录活性失效并损害糖酵解,从而诱导肿瘤缺氧核心中的PDAC细胞死亡。因此,USP25 / HIF-1α轴是PDAC中代谢重编程和存活的基本机制,可以进行治疗利用。
总之,该研究发现USP25是胰腺导管腺癌的潜在治疗靶点。
参考文献:
Nelson, J.K., Thin, M.Z., Evan, T. et al. USP25 promotes pathological HIF-1-driven metabolic reprogramming and is a potential therapeutic target in pancreatic cancer. Nat Commun 13, 2070 (2022). https://doi.org/10.1038/s41467-022-29684-9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Nat#
33
#治疗靶点#
50
#科学家发现#
53
#COMMUN#
50
#心血管#
61
又可以搞一批药了
46