Circulation:三支血管或左主干冠脉病变患者血运重建后的10年全因死亡率
2021-07-22 Nebula MedSci原创
如果三支血管同时病变的患者通过PCI不可能实现完全(或接近完全)血运重建,则应考虑采用CABG治疗
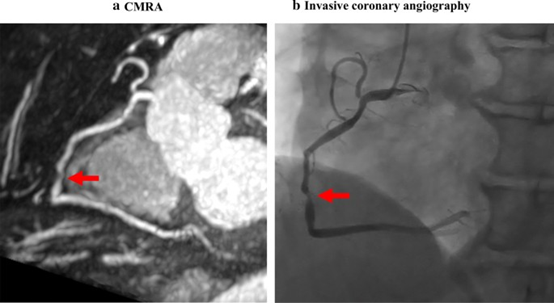
三支冠状动脉同时病变或左主干冠状动脉病变的患者,接受经皮冠状动脉介入治疗 (PCI) 或冠状动脉旁路移植术 (CABG) 后根据不完全血运重建 (IR) 和完全血运重建 (CR) 的10年全因死亡还没有完全明确。
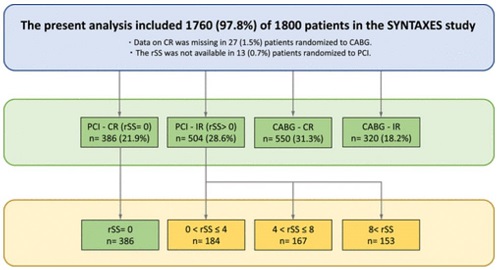
SYNTAX 延长生存期研究评估了最初参加 SYNTAX 试验的患者长达 10 年的生存状态。在本子研究中,研究人员将CABG CR 组的结果与 CABG IR、PCI CR 和 PCI IR 组的结果进行了比较。此外,在 PCI 队列中,采用了残差 SYNTAX 评分 (rSS) 量化 IR 的程度并评估其与致命性晚期结果的关联。rSS 为 0 表示 CR,而 rSS>0 表示 IR。
研究流程
IR更常见于接受PCI治疗的患者(PCI vs CABG:56.6% vs 36.8%);此外,无论是在PCI组还是CABG组,IR还更常见于三支血管病变的患者(与左主干病变患者相比:PCI组 58.5% vs 53.8%;CABG组 42.8% vs 27.5%)。与接受 CABG 的患者相比,接受 PCI 并 CR 的患者在 10 年全因死亡率方面没有显著差异。(PCI-CR vs CABG-IR vs CABG-CR:22.2% vs 24.3% vs 23.8%)。相反,接受 PCI 并 IR 的患者的10年全因死亡风险明显高于接受 CABG 治疗并 CR 的患者(33.5% vs 23.7%;校正风险比 1.48)。
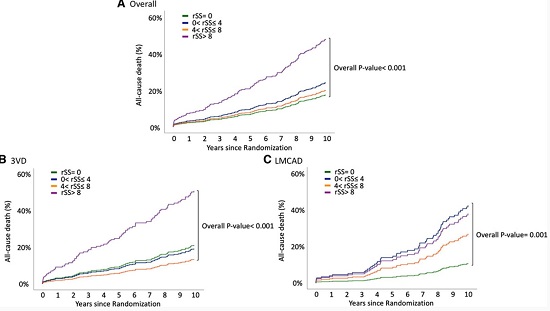
根据rSS分组的10年全因死亡率
根据 rSS 对 PCI 患者进行分层时,rSS≤8 的患者在 10 年全因死亡方面与其他三分位数的患者没有显著差异(rSS=0 vs rSS>0-4 vs rSS>4-8: 22.2% vs 23.9% vs 28.9%),但rSS>8的患者的10年全因死亡风险显著高于 CR 患者(50.1% vs 22.2%;校正风险比 3.40)。
综上所述,在PCI后,不完全血运重建常见,而且不完全重建的程度与患者的10年死亡率相关。如果三支血管同时病变的患者通过PCI不可能实现完全(或接近完全)血运重建,则应考虑采用CABG治疗。
原始出处:
Kuniaki Takahashi, et al. Ten-Year All-Cause Death According to Completeness of Revascularization in Patients With Three-Vessel Disease or Left Main Coronary Artery Disease: Insights From the SYNTAX Extended Survival Study. Circulation. 2021;144:96–109
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#左主干#
44
#冠脉病变#
42
#冠脉病#
43
#全因死亡率#
31
学习!
58
很好!
67
很好
59