Lancet oncol:卡巴他赛联合卡铂治疗去雄耐受性的转移性前列腺癌
2019-09-10 MedSci MedSci原创
在单组临床研究中,紫杉醇-铂联合治疗去势耐药的转移性前列腺癌显示出良好的活性,但尚无相关随机试验。研究人员开展一个1/2期开放性随机试验,招募进展期的去雄耐受性的转移性前列腺癌患者,评估卡巴他赛联合卡铂是否可提高这类患者的预后。1期目的是明确最大耐受剂量和剂量限制性毒性,2期评估无进展存活期。2012年8月17日-2015年5月11日,9位患者如期完成了1期试验,随后2期160位患者被随机分至卡巴
研究人员开展一个1/2期开放性随机试验,招募进展期的去雄耐受性的转移性前列腺癌患者,评估卡巴他赛联合卡铂是否可提高这类患者的预后。1期目的是明确最大耐受剂量和剂量限制性毒性,2期评估无进展存活期。
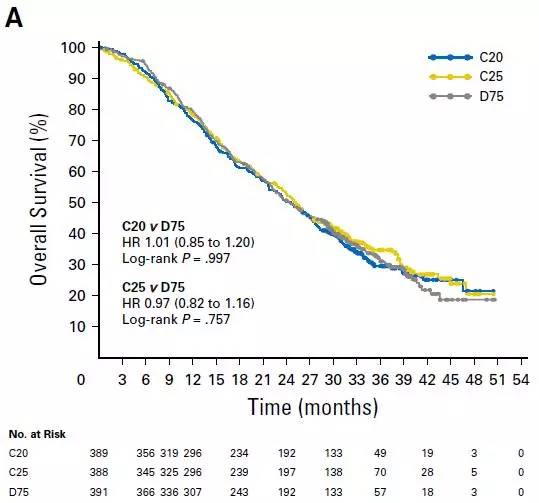
2012年8月17日-2015年5月11日,9位患者如期完成了1期试验,随后2期160位患者被随机分至卡巴他赛组(79位)或卡巴他赛联合卡铂组(81位)。在1期过程中,3级副反应事件有贫血(2例)、疲劳(1例)、血小板减少症(1例)、低镁血症(1例)、腹泻(1例)、低钾血症(1例)、厌食(1例)和脱水(1例),无4级副反应事件发生。无剂量限制性毒性,因此,最大耐受剂量定为卡巴他赛 25mg/m2、AUC的卡铂 4mg/ml·min,用于2期试验。中位随访31个月(IQR 20.5-37.1)时,联合组将中位无进展存活期从4.5个月(95% CI 3.5-5.7)延长至7.3个月(5.5-8.5;风险比0.69,95% CI 0.50-0.95,p=0.018).在2期研究中,最常见的3-5级副反应事件有疲劳(卡巴他赛组 vs 联合组:7例[9%] vs 16例[20%])、贫血(3[4%] vs 19[23%])、中性粒细胞减少(3[4%] vs 13[16%])、血小板减少症(1[1%] vs 11[14%])。无治疗相关死亡。
对于去雄耐受性转移性前列腺癌患者,与单用卡巴他赛相比,卡巴他赛联合卡铂可提高临床治疗效果。联合治疗的副反应事件发生率较高,但总体耐受性尚可。
原始出处:
Paul G Corn,et al.Cabazitaxel plus carboplatin for the treatment of men with metastatic castration-resistant prostate cancers: a randomised, open-label, phase 1–2 trial.The Lancet Oncology. September 09, 2019. https://doi.org/10.1016/S1470-2045(19)30408-5
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#铂#
24
#Oncol#
16
#Lancet#
28
#转移性#
39
#转移性前列腺癌#
26
#卡铂#
24
#耐受性#
23
谢谢梅斯分享这么多精彩信息
34
前列腺癌相关研究,学习了,谢谢梅斯
49