Blood:CBL突变通过强化LYN与PIK3R1相互作用驱动PI3K/AKT信号
2021-01-08 MedSci原创 MedSci原创
无偏移磷酸化蛋白质组学和相关作用组学突显了LYN激酶在突变型CBL蛋白致癌功能中的关键作用;LYN过度激活可加强CBL突变型细胞系和患者来源CMML细胞对达沙替尼的敏感性。
CBL编码E3泛素连接酶和信号转导接头,可调节受体和非受体酪氨酸激酶。复发性CBL突变可选择地破坏蛋白质的E3泛素连接酶活性,发生于髓系肿瘤,包括10-20%的慢性粒细胞单核细胞白血病(CMML)。CBL突变与患者不良预后有关,但是CBL突变的致癌机制和对治疗的意义尚不完全清楚。
Belizaire等结合功能检测和整体质谱来定义一组表达等位基因的CBL突变的细胞系中的磷酸化蛋白质组、CBL相互作用组和信号激活机制。
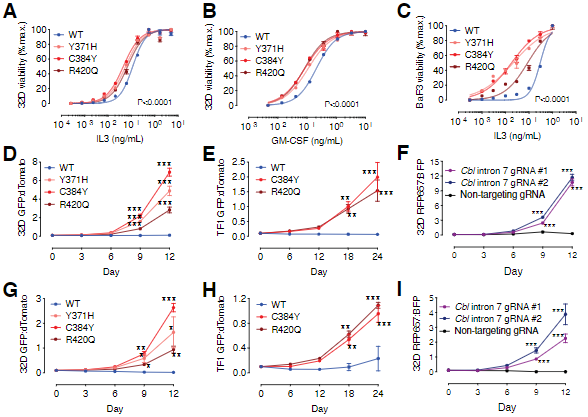
CBL功能获得性突变与白介素敏感性和LYN与PI3K/ AKT激活增强相关
LYN促进CBL-PIK3R1互作、增强CBL突变细胞的增殖
该研究分析表明,LYN激活增强和与突变型CBL的相互作用都是CBL突变细胞中CBL磷酸化增强、PIK3R1募集和下游PI3K/ AKT信号传导的关键驱动力。CBL的信号衔接子结构域,包括酪氨酸激酶结合结构域,脯氨酸富集区域和C末端磷酸酪氨酸位点,均是CBL突变发挥致癌功能所必需的。
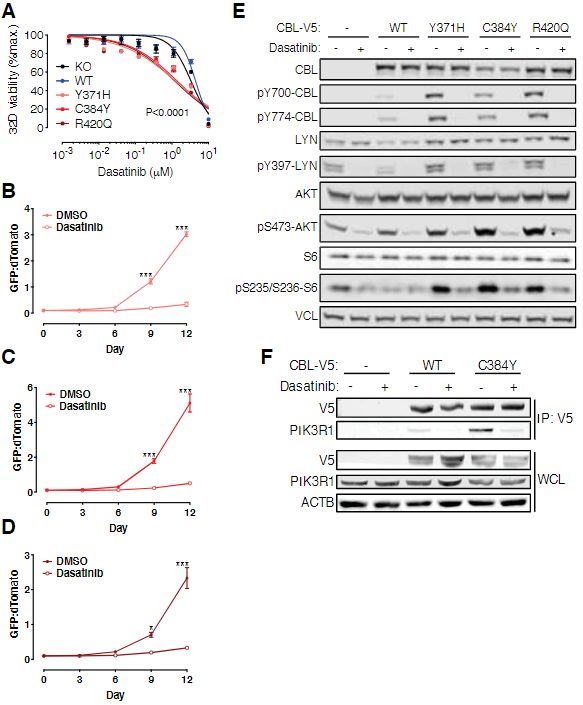
达沙替尼可抑制CBL突变细胞的增殖、CBL磷酸化、PI3K/ AKT信号及CBL-PIK3R1互作
遗传消融和达沙替尼(dasatinib)介导的LYN抑制可减少CBL磷酸化、CBL-PIK3R1相互作用和PI3K/AKT信号。此外,研究人员还证实,无论是在体内还是体外,达沙替尼对CBL突变细胞系和原发CMML都具有抗增殖活性。
综上所述,该研究对CBL突变分子功能机制的解析为探索LYN抑制在CBL突变型髓样恶性肿瘤中的治疗潜力提供了理论依据
原始出处:
Roger Belizaire, et al. CBL mutations drive PI3K/AKT signaling via increased interaction with LYN and PIK3R1. Blood. January 07, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Akt#
48
#相互作用#
46
#PI3K/AKT#
37
#PI3K#
44
#互作#
29
#PI3K/Akt信号#
31