JCEM:睾丸激素治疗对男性骨微结构和骨密度的影响
2021-03-22 MedSci原创 MedSci原创
50岁以上男性,睾丸激素治疗2年主要是通过影响皮层骨,使骨密度增加。降低骨折风险的意义需要进一步研究。
睾丸激素治疗可增加性腺功能减退男性的骨密度(BMD)。近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,研究人员旨在明确睾丸激素治疗对经高分辨率外周定量计算机断层扫描(HR-pQCT)评估的骨骼微结构的影响。

研究人员从澳大利亚6个研究中心招募了年龄超过50岁的男性。在社区生活方式计划的背景下,在两年内注射了癸酸睾丸激素或安慰剂。

该研究的主要终点为胫骨远端的皮质容积性BMD(vBMD),经HR-pQCT进行测量了177名男性(一个中心)。次要终点包括其他HR-pQCT参数和骨重塑标志物。研究人员通过双能量X射线吸收法(DXA)对601名男性(五个中心)测量了面积性BMD(aBMD)。研究人员使用线性混合模型进行重复测量,将两组之间在12和24个月时的平均调整差异(MAD)[95%CI]报告为治疗效果。
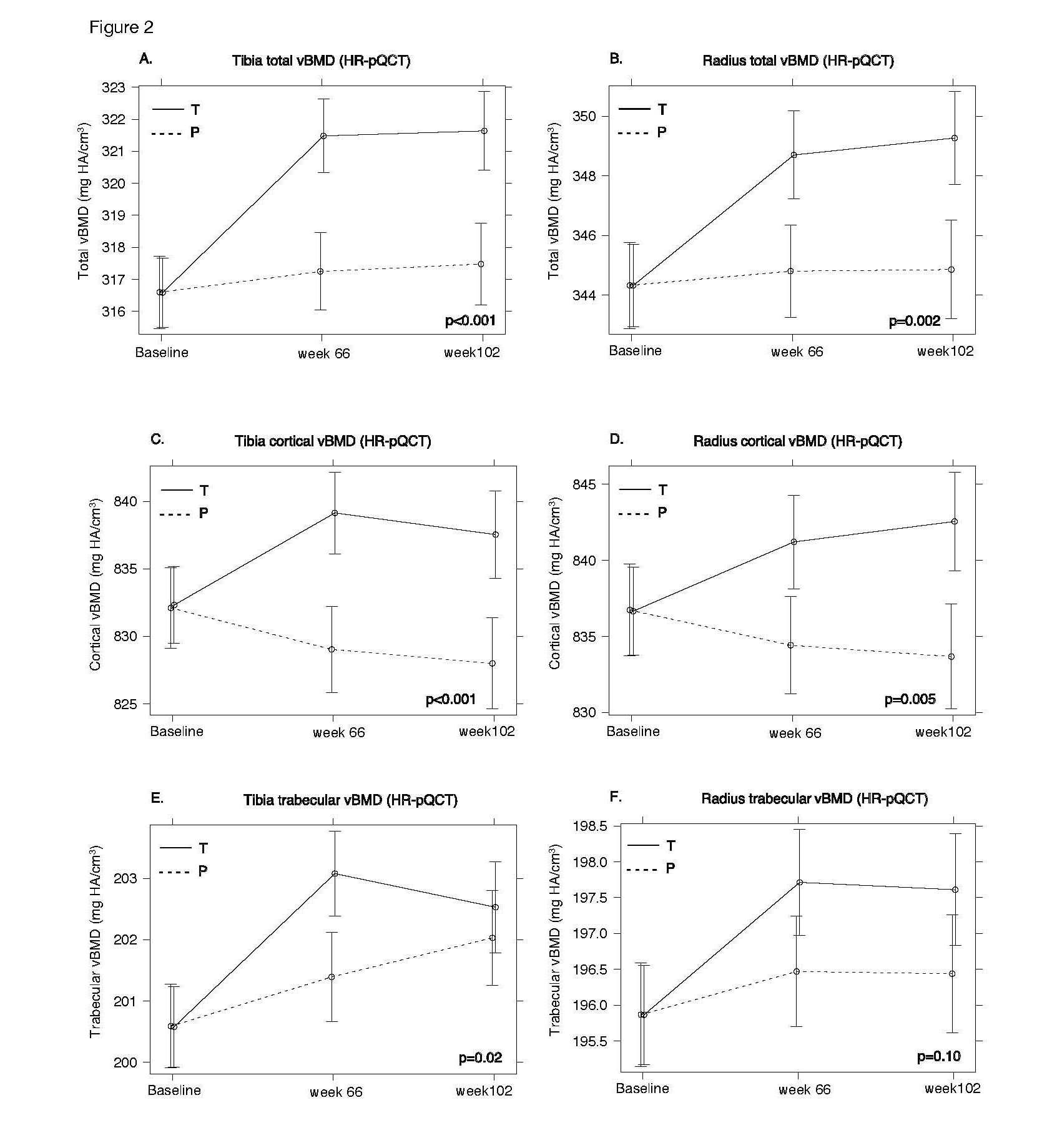
与安慰剂相比,在24个月内,睾丸激素治疗增加了胫骨皮质vBMD,9.33mgHA/cm3 [3.96; 14.71],p<0.001或3.1%[1.2; 5.0],桡骨vBMD,8.96mgHA /cm3 [3.30; 14.62],p=0.005或2.9%[1.0;4.9],总的vBMD,4.16mgHA/cm3[2.14; 6.19],p<0.001或1.3%[0.6; 1.9],总桡骨vBMD,4.42mgHA/cm3 [1.67; 7.16],p=0.002或1.8 %[0.4; 2.0]。睾丸激素还显著增加了两个部位的皮质面积和厚度。但对小梁结构的影响很小。睾丸激素可降低骨重塑标志物CTX,-48.1ng/L [-81.1;-15.1],p<0.001,P1NP,-6.8μg/L [-10.9;-2.7],p<0.001。睾丸激素显著提高腰椎的aBMD为0.04 g/cm2 [0.03; 0.05],p<0.001,以及总髋关节的aBMD为0.01g/cm2 [0.01; 0.02],p<0.001。
由此可见,50岁以上男性,睾丸激素治疗2年主要是通过影响皮层骨,使骨密度增加。降低骨折风险的意义需要进一步研究。
原始出处:
Mark Ng Tang Fui.et al.Effect of Testosterone treatment on bone microarchitecture and bone mineral density in men: a two-year RCT.JCEM.2021.https://pubmed.ncbi.nlm.nih.gov/33693907/
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#睾丸激素#
30
#微结构#
29
#JCEM#
34
#JCE#
30
#激素治疗#
40
#睾丸#
57
学习
83
学习了
75