Neoplasia:HECTD3至少部分通过稳定MALT1来促进癌细胞存活
2013-02-07 昆明动物研究所 Neoplasia
癌症治疗目前最大的挑战之一是肿瘤细胞具有原发的耐药性以及治疗后逐渐产生抗药性。顺铂是目前广泛用于临床治疗乳腺癌、卵巢癌、前列腺癌等实体瘤的化疗药物,它通过造成DNA损伤诱导细胞凋亡杀死癌细胞。但是癌细胞抗药的分子机制还不是很清楚。 泛素化是一种蛋白质的翻译后修饰,参与调控多种生物学过程,其系统功能紊乱与癌细胞凋亡以及癌症发展进程中起到了关键作用。蛋白泛素化过程由三种酶依次催化完成,包括泛素激活酶
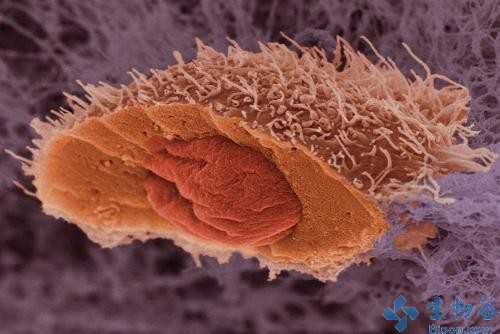
癌症治疗目前最大的挑战之一是肿瘤细胞具有原发的耐药性以及治疗后逐渐产生抗药性。顺铂是目前广泛用于临床治疗乳腺癌、卵巢癌、前列腺癌等实体瘤的化疗药物,它通过造成DNA损伤诱导细胞凋亡杀死癌细胞。但是癌细胞抗药的分子机制还不是很清楚。
泛素化是一种蛋白质的翻译后修饰,参与调控多种生物学过程,其系统功能紊乱与癌细胞凋亡以及癌症发展进程中起到了关键作用。蛋白泛素化过程由三种酶依次催化完成,包括泛素激活酶(E1)、泛素连接酶(E2)和泛素连接酶(E3)。其中,E3泛素连接酶决定修饰底物的特异性。HECTD3 (Homologous to the E6-associated protein carboxyl terminus domain containing 3) 是一个功能未知的新的E3泛素连接酶。
2013年1月的癌症领域主流杂志NEOPLASIA发表了中国科学院昆明动物研究所陈策实研究员课题组的工作The HECTD3 E3 Ubiquitin Ligase Suppresses Cisplatin-induced Apoptosis via Stabilizing MALT1。该研究首次发现:在乳腺癌和宫颈癌细胞抑制E3泛素连接酶HECTD3表达后能让癌细胞对顺铂更加敏感,小鼠实验也充分证明了这一点。进一步研究发现,敲低HECTD3表达使癌细胞对紫杉醇以及放射治疗也更加敏感。
为了探索其分子机制,课题组利用酵母双杂交和免疫共沉淀实验发现,MALT1(mucosa-associated lymphoid tissue 1)是HECTD3的底物蛋白。HECTD3通过其N端DOC结构域与MALT1的DD结构域直接作用,然后促进MALT1泛素化修饰。有趣的是,这种泛素化修饰不像大多数情况下导致底物蛋白降解,相反地,使MALT1蛋白在顺铂存在的情况下更加稳定。这是因为HECTD3介导的MLAT1多聚泛素化链结构不是通过泛素分子传统的赖氨酸48位延伸,而是通过泛素分子其它赖氨酸残基延伸。
MALT1已知在淋巴细胞的NF-kB信号通路活化中扮演重要角色,但是在实体瘤中的角色还没有任何研究。该研究首次发现在实体癌细胞中敲低MALT1表达能够增强顺铂诱导的细胞凋亡。这个功能虽然比敲低HECTD3微弱一些,但是足以说明MALT1和HECTD3的抑制细胞凋亡功能基本一致。相反,过表达MALT1则能抑制细胞凋亡并挽救敲低HECTD3引起的顺铂敏感性增加。
此项研究表明,HECTD3至少部分通过稳定MALT1来促进癌细胞存活。这些结果为克服癌症治疗抗性提供了新的治疗策略。
该研究项目得到了国家自然科学基金,科技部蛋白质重大研究计划以及云南省高端科技人才项目的资助。

DOI 10.1593/neo.121362
PMC:
PMID:
The HECTD3 E3 Ubiquitin Ligase Suppresses Cisplatin-induced Apoptosis via Stabilizing MALT1
Yi Li*,†,3, Xi Chen*,‡,3, Zehua Wang*, Dong Zhao§, Hui Chen¶, Wenlin Chen#, Zhongmei Zhou*, Junran Zhang**, Jing Zhang¶, Hongmin Li¶,†† and Ceshi Chen*
Homologous to the E6-associated protein carboxyl terminus domain containing 3 (HECTD3) is an E3 ubiquitin ligase with unknown functions. Here, we show that HECTD3 confers cancer cell resistance to cisplatin. To understand the molecular mechanisms, we performed a yeast two-hybrid analysis and identified mucosa-associated lymphoid tissue 1 (MALT1) as an HECTD3-interacting protein. HECTD3 promotes MALT1 ubiquitination with nondegradative polyubiquitin chains by direct interacting with the MALT1 through its N-terminal destruction of cyclin domain. HECTD3 does not target MALT1 for degradation but stabilize it. HECTD3 depletion dramatically decreases the levels of MALT1 in MCF7 and HeLa cells treated with cisplatin, which is correlated to an increase in apoptosis. Knockdown of MALT1 likewise increases cisplatin-induced apoptosis in these cancer cells. However, HECTD3 overexpression leads to a decreased cisplatin-induced apoptosis, whereas overexpression of MALT1 partially rescues HECTD3 depletion–induced apoptosis. These findings suggest that HECTD3 promotes cell survival through stabilizing MALT1. Our data have important implications in cancer therapy by providing novel molecular targets.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ASIA#
37
#eCTD#
36
#ALT#
31
#癌细胞#
30