Frontiers:注意你的糖化!我国学者发现糖化升高影响冠心病支架植入结果!
2022-01-11 MedSci原创 MedSci原创
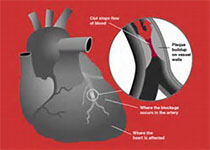
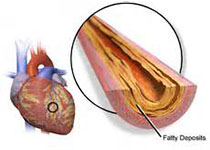
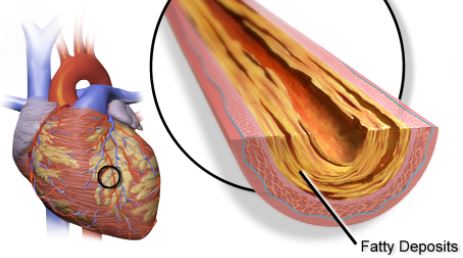
斑块脆弱性的增加和更高的脂质变异性是不良心血管事件的原因。
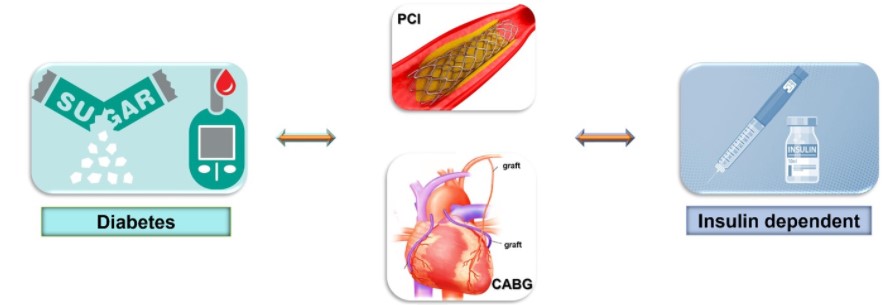
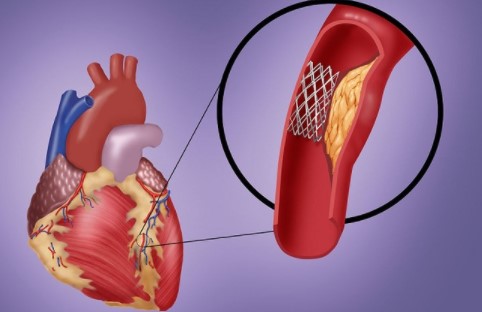
斑块脆弱性的增加和更高的脂质变异性是不良心血管事件的原因。尽管葡萄糖和脂质代谢密切相关,但糖化血红蛋白A1c(HbA1c)升高对斑块脆弱性和脂质变异性的影响仍不清楚。为此,我国福建医科大学和浙江大学的心血管专家开展了相关研究,结果发表在Frontiers in Cardiology Medicine杂志上。
在2009年至2019年接受经皮冠状动脉介入治疗(PCI)的受试者中,366名患者接受了血管内光学相干断层扫描(OCT)评估,4445名患者在PCI后1年内进行了预定的随访。通过OCT检查分析了罪魁祸首血管的脆弱性特征,包括评估脂质、巨噬细胞、钙质和最小纤维帽厚度(FCT)。
通过不同的定义,包括标准差(SD)、变异系数(CV)和独立于平均值的变异性(VIM),来确定各次访问的血脂变异性。多变量线性回归分析被用来验证HbA1c对斑块脆弱性特征和血脂变异性的影响。对非糖尿病患者也进行了探索性分析。
结果显示,在入选的受试者中,术前HbA1c为5.90±1.31%,平均随访HbA1c为5.98±1.16%。通过OCT评估,多变量线性回归分析表明,HbA1c升高的患者最小FCT更薄(β=-6.985,P=0.048),脂质指数(LI)更大(β=226.299,P=0.005),巨噬细胞指数更高(β=54.526,P=0.045),提示斑块易损易破裂。
即使在非糖尿病患者中,HbA1c的升高也会线性地降低最小FCT(β=-14.011,P=0.036),增加LI(β=290.048,P=0.041)和巨噬细胞指数(β=120.029,P=0.048)。
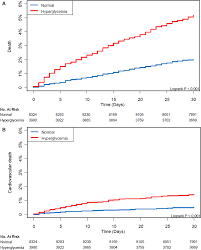
随后,在PCI术后1年内进行了定期随访。多变量线性回归分析证明,平均随访HbA1c水平的升高会增加血脂谱的VIM,包括低密度脂蛋白胆固醇(β=2.594,P<0. 001),高密度脂蛋白胆固醇(β=0.461,P=0.044),非高密度脂蛋白胆固醇(β=1.473,P<0.001),总胆固醇(β=0.947,P<0.001),和甘油三酯(β=4.217,P<0.001)。这一结果在非糖尿病患者中是一致的,当用SD和CV来估计变异性时也得到了验证。
由此可见,在接受选择性PCI的患者中,HbA1c的升高会增加动脉粥样硬化斑块的脆弱性和血脂谱的逐次变化,且该结果在非糖尿病患者仍可靠。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#我国学者#
38
#ERS#
41
#支架植入#
55
#植入#
43
学习了
78
学习了
70