Oncogene:钙调素促进前列腺癌休眠
2020-12-31 AlexYang MedSci原创
前列腺癌是男性死亡的主要原因之一。前列腺癌患者死亡的主要原因可归结为疾病的转移扩散或初始治疗后的肿瘤复发。前列腺肿瘤发展成为局部或远处部位可见肿瘤之前,长期处于不能检测到或休眠状态。然而,休眠的分子机
前列腺癌是男性死亡的主要原因之一。前列腺癌患者死亡的主要原因可归结为疾病的转移扩散或初始治疗后的肿瘤复发。前列腺肿瘤发展成为局部或远处部位可见肿瘤之前,长期处于不能检测到或休眠状态。然而,休眠的分子机制尚不清楚。
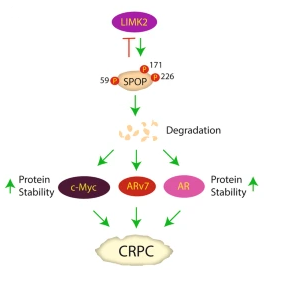
最近,有研究人员进行了基因表达差异分析,并发现了一个促进前列腺癌休眠的基因Regucalcin(RGN)。研究发现,RGN表达水平较高的癌症患者的无复发和总体生存期明显延长。利用多西环素诱导的RGN表达系统,研究人员发现RGN在前列腺肿瘤细胞中的异位表达诱导了体内休眠,而抑制RGN后则引发了肿瘤的复发生长。另一方面,在LNCap细胞中沉默RGN可促进其在小鼠胫骨中的外生长。重要的是,RGN促进多个已知的肿瘤休眠标记,包括p38 MAPK的激活、Erk信号的减少和FOXM1表达的抑制。此外,研究人员发现RGN通过增加外泌体中miR-23c分泌水平,能够显著抑制血管生成。有趣的是,他们发现FOXM1对前列腺癌中miR-23c的表达存在负调控。另外,研究人员还发现了11个RGN下游靶基因,它们能独立预测患者更长的无复发生存期,且这些基因的表达受到FOXM1和/或p38 MAPK的调控。
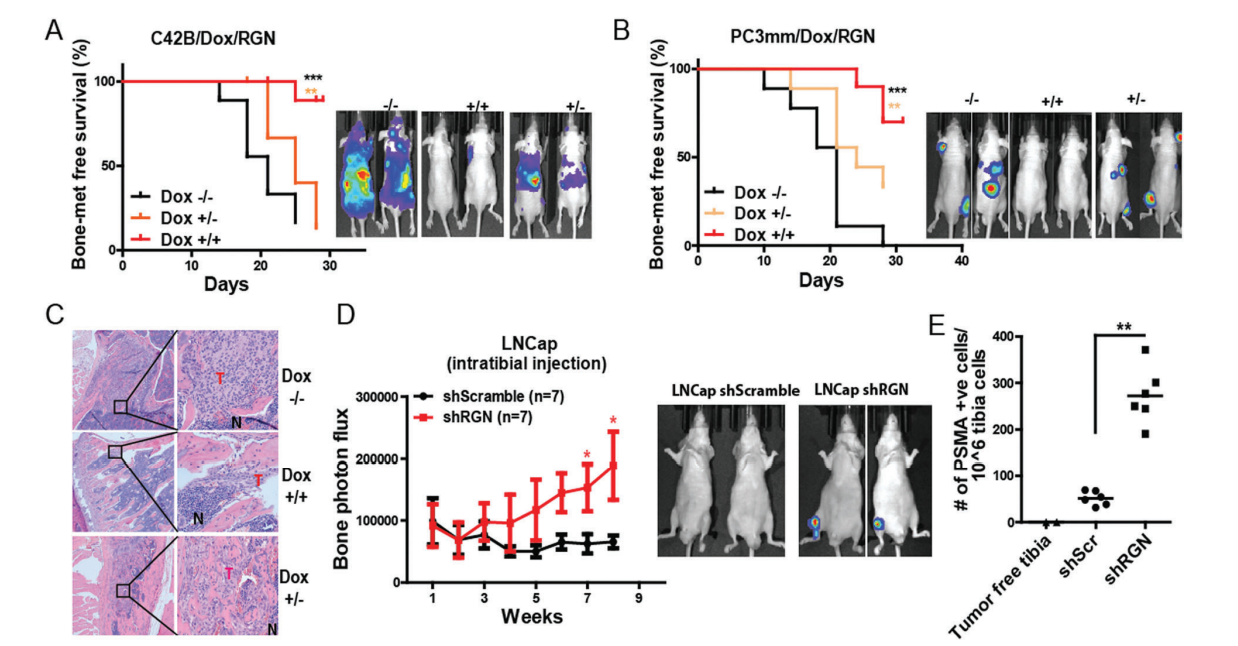
体内试验中RGN促进休眠
最后,研究人员指出,他们的发现表明RGN在前列腺癌休眠中发挥了关键作用,且RGN信号传导和外泌体miR-23c可作为预测复发的生物标志物。
原始出处:
Sambad Sharma, Xinhong Pei, Fei Xing et al. Regucalcin promotes dormancy of prostate cancer. Oncogene. Dec 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#休眠#
32
#Gene#
28
学习了
65
#Oncogene#
38
前列腺癌相关研究,学习了,谢谢梅斯
42