病例报告:抗CD6抗体治疗COVID-19病人细胞因子释放综合征
2021-09-23 MedSci原创 MedSci原创
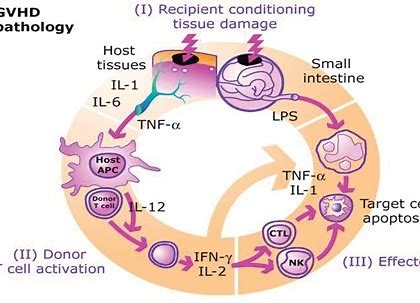
在COVID-19中,炎性细胞因子释放综合征与病情的进展有关。Itolizumab是一种单克隆抗体,可识别活化T细胞中表达的人CD6。该抗体已被证明可安全有效地治疗中度至重度银屑病。其作用与减少促炎细
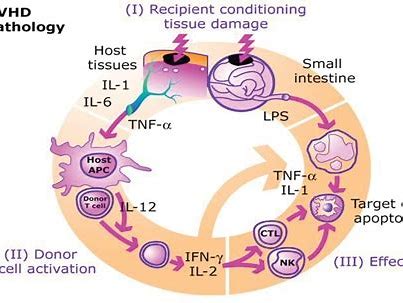
在COVID-19中,炎性细胞因子释放综合征与病情的进展有关。Itolizumab是一种单克隆抗体,可识别活化T细胞中表达的人CD6。该抗体已被证明可安全有效地治疗中度至重度银屑病。其作用与减少促炎细胞因子释放有关,包括IFN-γ、IL-6和TNF-α。
本篇文章报告了3例重度和重症COVID-19患者接受Itolizumab治疗(作为扩大用药方案的一部分)的结局。Itolizumab能够降低所有患者的IL-6浓度。
3例患者中有2例出现呼吸和放射学改善,完全恢复。
病例描述
病例1: 53岁女性患者,有原发性高血压和2型糖尿病个人史,表现为呼吸急促超过40 rpm、使用呼吸辅助肌肉组织和干咳症状。
初始气体测定显示中度低氧血症和呼吸性碱中毒,氧分压/吸入氧分数(PO2/FiO2)比值为191。胸部x线显示双肺野间质性病变。
患者开始洛匹那韦/利托那韦、氯喹、重组IFNα-2b和罗氏芬治疗。尽管进行了治疗,但疾病随后进展为低氧性呼吸衰竭,需要开始有创机械通气。
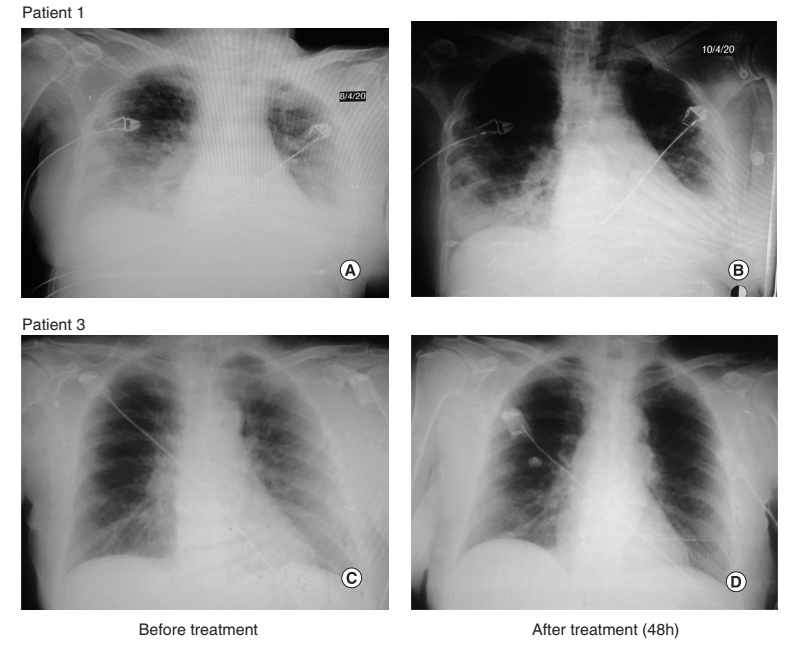
在入住ICU的第13天,患者显示间质性多灶性肺炎的放射学恶化,ALP、LDH、红细胞沉降率和D-二聚体升高。医生以200 mg的剂量给予Itolizumab。首次Itolizumab给药48h后,PO2/FiO2改善,并有放射学改善的证据(图1A和B)。
患者在抗体首次给药后拔管,其状态从危重变为重度。患者在首次输注后48h接受第二次抗体给药(200 mg)。首次给药后3天,患者血流动力学稳定,并接受自主通气。
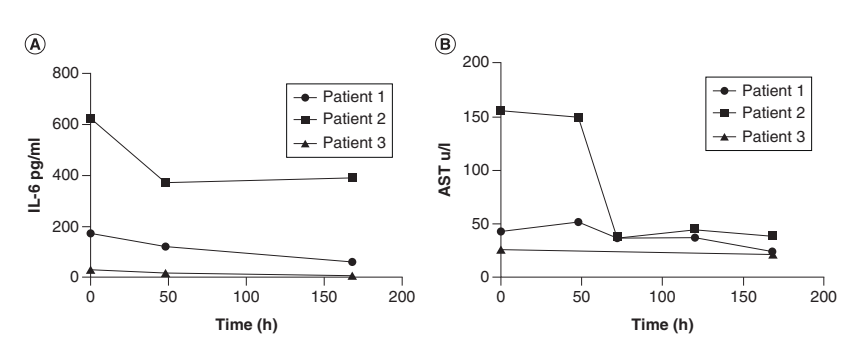
在Itolizumab给药前以及首次给药2天和7天后评价IL-6水平。如图2A所示,IL-6水平随时间从172 pg/mL降至60 pg/mL(第7天)。在相同的时间间隔评价IL-1,但检测不到。此外,在不同时间点评价了天冬氨酸氨基转移酶(AST)浓度,显示7天后从43 U/L降至24 U/L(图2B)。未报告与itolizumab相关的不良事件。
Figure 1:一剂Itolizumab单抗给药前后的放射学影像
病例2: 89岁男性患者,有慢性缺血性心脏病、永久性房颤、高血压和甲状腺功能减退个人史。既往有酗酒史,最近3个月因感染性呼吸道疾病多次住院。因气短、发热、乏力及干咳7天后于4月2日来院就诊。
体格检查显示呼吸衰竭体征,特征为心动过速、呼吸急促、肋间肌和锁骨上肌回缩、高血压、血氧饱和度82%、利尿不良和嗜睡。胸部x线检查显示双侧肺炎性浸润,主要见于右肺。
入院ECG显示房颤伴快速心室反应,初始气体测量显示重度低氧血症和呼吸性碱中毒。患者还出现白细胞增多、球状沉降速度改变以及AST、LDH、D-二聚体值升高和C反应蛋白阳性。患者入住ICU,需要有创机械通气。
开始洛匹那韦-利托那韦、氯喹、IFNα-2b、美罗培南和利奈唑胺治疗。入住ICU后3天,由于双侧肺浸润恶化以及通气功能恶化(PO2/FiO2 = 173),处方开始使用Itolizumab。首次抗体输注后,PO2/FiO2显著升高(PO2/FiO2 = 320),并有放射学改善的证据。3天后,患者显示左肺放射学恶化,表现为肺泡通气不足和肺不张。
患者在首次给药后72 h接受第二次单克隆抗体输注,而在第二次给药后2天,由治疗医生酌情给予第三次给药。总体而言,患者接受了3次Itolizumab (200 mg)给药,未发生任何相关不良事件。在Itolizumab给药前和首次给药后2、4和7天评价IL-6水平。基线时IL-6极高(623 pg/mL),尽管细胞因子水平降低约50%,但7天后最低值仍高于300 pg/mL。
IL-6动力学如图2A所示。除IL-6外,在疾病的该时间点检测不到IL-1。
有趣的是,对于AST,在第7天检测到显著降低(给药前:156 U/L,D7:40 U/L),如图2B所示。入住ICU 10天后,患者出现心肌功能障碍和休克,需要去甲肾上腺素血管活性支持。第13天,患者因混合性心血管和呼吸衰竭最终死亡。
病例3: 81岁女性患者,住院时未发现COVID-19阳性接触。她于4月2日开始出现症状,并于4月5日进入ICU。患者既往有高血压、糖尿病、青光眼病史和吸烟习惯。因频繁咳嗽、喘息及腹泻入院。4月7日,通过RT-PCR证实了通过COVID-19确诊的病毒性肺炎。
5 L/min的氧气支持和头孢曲松、洛匹那韦-利托那韦、氯喹和IFNα-2b治疗。胸部影像显示双肺双侧间质浸润。尽管患者不需要有创机械通气,但其病情被归类为重度。
患者入住ICU后第二天接受了Itolizumab (200 mg)给药。抗体给药后2天,连同其余治疗,呼吸窘迫改善,而胸部影像显示双肺肺泡间质浸润减少(图1 C和D)。患者在临床和影像学进展良好后离开ICU。
在抗体给药前后测定IL-6浓度。基线时的IL-6水平低于既往病例(30 pg/mL),但在输注itolizumab后48h和168h也降低(图2A)。抗体给药前和给药后48 h无法溯源IL-1和TNF-α。
关于AST浓度,治疗期间数值在正常范围内(图2B)。
Figure 2:患者血清中的循环生物标志物
结论
综上所述,在这些重症和危重患者中,itolizumab能够降低IL-6浓度。值得注意的是,未报告itolizumab相关不良事件。基线IL-6水平低于200 pg/mL的患者显示迅速的临床和放射学恢复。我们预计,及时使用这种抗炎抗体联合适当的抗病毒和抗凝治疗可以降低与COVID-19相关的病死率。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#胞因子#
31
#CD6#
37
#细胞因子#
48
#病例报告#
45
#综合征#
29