Am J Obstet Gynecol:埃索美拉唑能否延长未足月先兆子痫女性的妊娠时间?
2018-11-20 吴星 环球医学
未足月先兆子痫的致命死亡率或残疾率较高。除了分娩之外,尚无延缓这种疾病的疗法。临床前研究发现质子泵抑制剂可能有效。2018年10月,发表在《Am J Obstet Gynecol》的一项双盲、随机对照试验考查了,埃索美拉唑能否延长确诊未足月先兆子痫女性的妊娠。
目的:考察埃索美拉唑能否延长确诊不足月先兆子痫女性的妊娠时间。
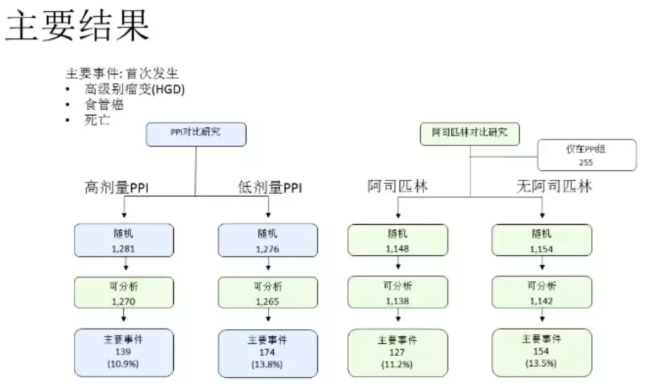
研究设计:研究者在南非泰格堡医院开展了一项双盲、随机对照试验。未足月先兆子痫女性(胎龄26周+0天至31周+6天)被随机分配至埃索美拉唑每日40 mg组或安慰剂组。首要结局指标为孕龄延长5天。次要结局指标为母体和新生儿结局。研究者比较了与先兆子痫相关的血管内皮功能紊乱的循环标记物,并开展了药代动力学研究。
结果:2016年1月至2017年4月,研究者招募120例受试者。1例患者因为错误随机化被排除,剩下的受试者随机分配至埃索美拉唑组(59例),安慰剂组(60例)。纳入时的中位胎龄为29周+4天。从随机化至分娩期间,中位时间无组间差异:埃索美拉唑组11.4天(四分位间距,3.6~19.7天),安慰剂组8.3天(四分位间距,3.8~19.6)(埃索美拉唑组进一步延长3天;95%置信区间,–2.9~8.8;P=0.31)。埃索美拉唑组无胎盘早剥,安慰剂组发生6例胎盘早剥(校正P=0.01,P=0.14)。其他母体或新生儿结局或血管内皮功能紊乱标记物没有差异。在使用埃索美拉唑治疗的女性母体的血液中监测到了埃索美拉唑及其代谢物,但脐带血中只有微量。
结论:每日埃索美拉唑40 mg不会延长未足月先兆子痫女性的妊娠时间,或降低体循环中可溶FMS样酪氨酸激酶1浓度。或需要更高母体循环水平以发挥临床疗效。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#NEC#
0
#TET#
37
#妊娠时间#
39
#埃索美拉唑#
42