European Radiology:平扫和延迟期可以提高动脉CTA对活动性下消化道出血的诊断
2022-05-01 MedSci原创 MedSci原创
CTA能提供详细的血管解剖和出血定位,有助于规划经导管治疗,并减少手术时间、透视辐射暴露和手术对比剂剂量。
下消化道出血(LGIB)是急诊科就诊和住院的一个常见原因,每年的发病率为20.5-36.0/10万。据报道,入院时出现的LGIB的死亡率为2.4%,住院期间出现的死亡率高达23.1%。
以前,99mTc标记的红细胞闪烁术因其高灵敏度而被普遍用于LGIB的检查。然而,由于CTA能够以与闪烁术相当的速度(低至0.3 mL/min)发现活动性出血,其敏感性和特异性高,因此在许多机构中已被CT血管成像(CTA)所取代。此外,CTA能提供更详细的血管解剖和出血定位,这可能有助于规划经导管治疗,并减少手术时间、透视辐射暴露和手术对比剂剂量。然而,尽管多期相CTA有很多优点,但这些优点都是理论上的,必须与缺点进行权衡。
近日,发表在European Radiology杂志的一项研究评估了包含额外的平扫和延迟期的多期相CTA在评估LGIB方面的价值,明确了额外期相是否会影响LGIB检测的敏感性和特异性,并评估了阅读时间和观察者之间是否存在血管外渗和出血位置的一致性。

本研究采用随机实验区块设计,3名受过介入放射学专业培训的盲目放射学家回顾性地解释了2012年10月至2017年10月期间完成的96次CTA检查,使用了(1)仅动脉期、(2)动脉期/平扫以及(3)动脉期/平扫/延迟期相匹配。证实为阳性和阴性的LGIB研究被匹配、平衡和随机排序。评估了敏感性、特异性、阳性似然比、阴性似然比、阳性和阴性预测值以及确定存在/不存在活动性出血的时间,采用广义估计方程(GEE)与三明治估计法假设二元分布来估计相位配置之间诊断性能的相对效益。
特异性随着期相的增加而增加(动脉期72.2;动脉期/平扫86.1;动脉/平扫/延迟期95.1;P < 0.001),而敏感性没有变化(动脉77.1;动脉/平扫70. 2;动脉期/平扫/延迟期73.1;p = 0.11)或每次研究识别出血所需的平均时间(s,动脉期34.8;动脉期/平扫33.1;动脉期/平扫/延迟期36.0;p = 0.99)。阅读者之间的总体一致性(Kappa)同样增加(动脉0.47;动脉期/平扫0.65;动脉期/平扫/延迟期0.79)。
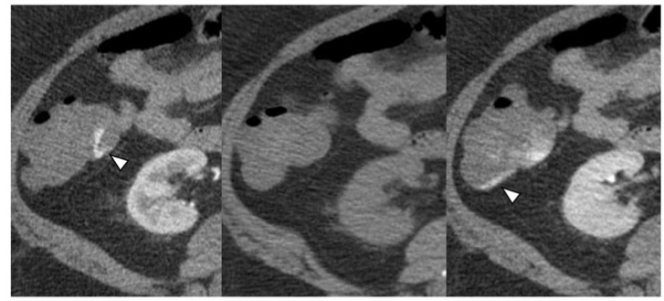
图 轴位三期相CTA显示的憩室出血,随后在结肠镜检查中得到确认。动脉期的活动性外渗(左)没有与平扫期的关联(中),并在延迟图像上发展(右)
本研究结果表明使用三期相CTA可提高LGIB的诊断准确率。在动脉期CT血管造影的基础上使用平扫和延迟期,可提高了特异性和阅读者之间的整体一致性,也没有降低敏感性或提高每次阅读的时间。
原文出处:
Matthew E Pouw,Joseph W Albright,Meagan J Kozhimala,et al.Adding non-contrast and delayed phases increases the diagnostic performance of arterial CTA for suspected active lower gastrointestinal bleeding.DOI:10.1007/s00330-022-08559-z
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CTA#
46
#PE#
56
#活动性#
60
#下消化道出血#
54
#消化道#
45