European Radiology:CTA自动侧支评分算法的诊断性能
2022-06-12 shaosai MedSci原创
快速、可靠、一致的自动评分不仅可以减少启动治疗前的时间延迟,还可以减少人为的判断错误,从而改善治疗效果。
 众所周知,血管内治疗(EVT)是颅内大血管闭塞导致的缺血性卒中患者的首选治疗方案。EVT后的临床预后受患者特征、工作流程参数和影像学参数的影响。预测预后的一个重要影像学参数是为缺血区提供血液供应的侧支循环的程度,可用来从血管内治疗中获益的患者进行筛选。传统的侧支评分系统使用的是基于评估受影响和未受影响半球之间大脑中动脉(MCA)区域血管充盈的视觉差异分类量表。然而,由放射科医生或卒中医生评估的视觉副损伤评分(vCS)在观察者之间和内部有很大的差异。
众所周知,血管内治疗(EVT)是颅内大血管闭塞导致的缺血性卒中患者的首选治疗方案。EVT后的临床预后受患者特征、工作流程参数和影像学参数的影响。预测预后的一个重要影像学参数是为缺血区提供血液供应的侧支循环的程度,可用来从血管内治疗中获益的患者进行筛选。传统的侧支评分系统使用的是基于评估受影响和未受影响半球之间大脑中动脉(MCA)区域血管充盈的视觉差异分类量表。然而,由放射科医生或卒中医生评估的视觉副损伤评分(vCS)在观察者之间和内部有很大的差异。
快速、可靠、一致的自动评分不仅可以减少启动治疗前的时间延迟,还可以减少人为的判断错误,从而改善治疗效果。近日,发表在European Radiology杂志的一项研究评估了一种市售的评估急性缺血性卒中患者基线CTA图像侧枝得分算法的性能,为临床早期识别该类患者并进行早期治疗提供了支持。
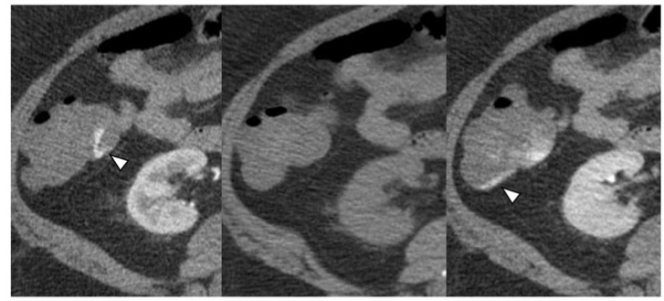
本研究回顾性地评估了MR CLEAN注册中心(n = 1627)的颅内颈动脉(ICA)、大脑中动脉M1或M2段闭塞的基线CTA扫描图像(层厚≤3毫米)。所有CTA扫描都由8位专家放射学家(参考标准)进行视觉CS(0-3)评估。基于网络的人工智能算法对正确检测到的闭塞侧的侧支循环进行量化(0-100%)。评估了视觉CS和分类的自动CS(0:0%,1:>0-≤50%,2:>50-<100%,3:100%)之间的一致性。计算了将患者分为良好(CS:2-3)和不良(CS:0-1)的曲线下面积(AUC)值,以及预测功能独立(90天改良Rankin量表0-2)的值。并报告了造影剂使用后CTA采集时间的影响。
在分析的扫描中(n = 1024),发现视觉CS和自动CS之间有59%的一致性。辨别良好与不良CS的AUC为0.87(95%CI:0.85-0.90)。CTA采集的时间并不影响判别性能。自动CS预测功能独立的AUC为0.66(95% CI 0.62-0.69),与视觉CS 0.64(95% CI 0.61-0.68)相似。
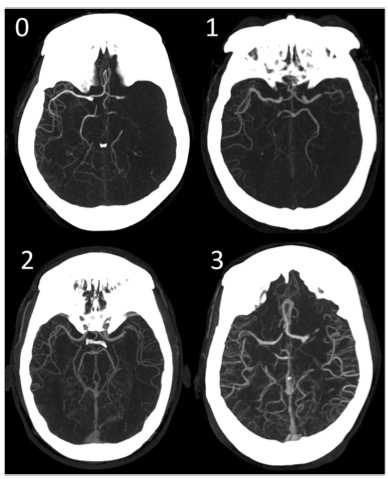
图 M1闭塞患者的侧支循环视觉评分分级。0:无侧支循环,闭塞区域0%的填充。1: 极少的侧支循环,>0%和≤5 0%的闭塞区被填充。2: 中等程度的侧支循环,闭塞区域的填充率>50%,<100%。3:良好的侧支循环,闭塞区100%被填塞
本研究表明,这种基于深度学习的侧支循环自动评分算法在对大血管闭塞的急性缺血性卒中患者进行良好与不良侧支循环评分的分类以及预测功能独立性方面表现出与放射科专家相似的诊断性能。
原文出处:
Lennard Wolff,Simone M Uniken Venema,Sven P R Luijten,et al.Diagnostic performance of an algorithm for automated collateral scoring on computed tomography angiography.DOI:10.1007/s00330-022-08627-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CTA#
55
#PE#
40
#诊断性#
41
学习
55