European Radiology:CTA与Agatston评分对冠心病稳定胸痛患者的诊断价值
2022-07-07 shaosai MedSci原创
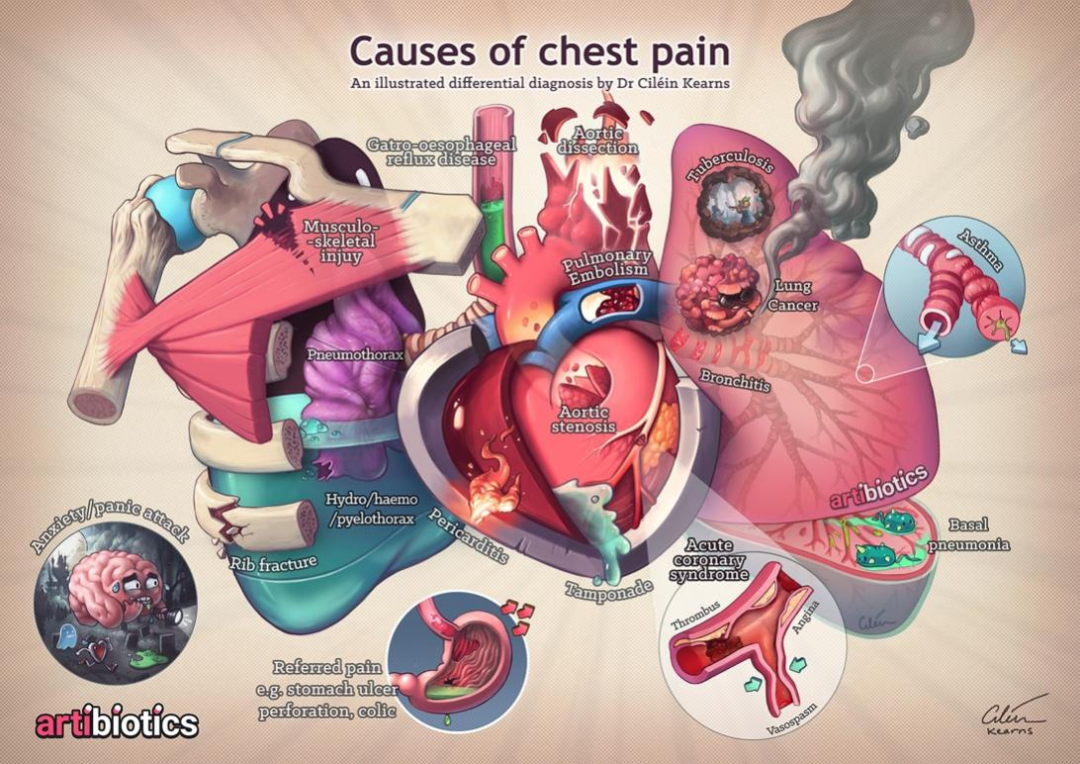
众所周知,CTA 在检测稳定性胸痛患者的阻塞性 CAD 方面显示出良好的诊断准确性。
 冠状动脉钙化(CAC)已成为检测冠状动脉疾病(CAD)严重程度的独立诊断指标,最常用的量化方法是Agatston评分法,CAC定量评估常用于无症状患者的风险分层。
冠状动脉钙化(CAC)已成为检测冠状动脉疾病(CAD)严重程度的独立诊断指标,最常用的量化方法是Agatston评分法,CAC定量评估常用于无症状患者的风险分层。
CORE-64国际多中心研究显示,CTA对CAC升高超过600的患者的诊断准确性明显降低。众所周知,CTA 在检测稳定性胸痛患者的阻塞性 CAD 方面显示出良好的诊断准确性。由于 Agatston 评分与 CTA 的比较诊断准确性存在相互矛盾,因此Agatston 评分在检测阻塞性 CAD 中的诊断价值仍不明确。
近日,发表在European Radiology杂志的一项研究通过使用来自全球协作性COME-CCT联盟分析,进一步明确了 CTA 的诊断准确性是否受到较高 Agatston 评分的影响,为对冠心病患者进行准确的风险分层提供了参考依据。
析(COME-CCT)联盟共纳入了2452名有稳定胸痛并有临床指征的疑似CAD的侵入性冠状动脉造影(ICA)患者。Agatston评分>400被认为是阳性,阻塞性CAD被定义为ICA上冠状动脉直径狭窄至少50%,被用作参考标准。
44.9%的患者(1100/2452)被诊断为阻塞性CAD。Agatston评分的中位数为74。CTA检测阻塞性CAD的诊断准确性(81.1%,95%置信区间[CI]:77.5至84.1%)明显高于Agatston评分(68.8%,95%CI:64.2至73.1%,P <0.001)。在Agatston评分为零的患者中,17%(101/600)有阻塞性CAD。CTA的诊断准确性在低至中度(1至<100,100-400)与中至高度Agatston评分(401-1000,>1000)的患者中没有明显差异。
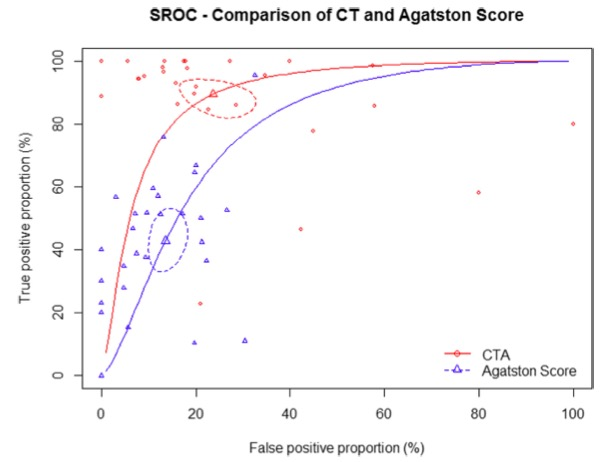
图 CTA和Agatston评分的SROC曲线
与Agatston评分相比,CTA在检测有稳定胸痛并有ICA临床指征的有症状患者的CAD方面显示出总体上更高的诊断准确性。这些发现适用于不同Agatston评分的患者,包括没有冠状动脉钙化的患者。此外,CTA的诊断准确性在中、高度Agatston评分的患者中诊断性能一致。
原文出处:
Viktoria Wieske,Mario Walther,Benjamin Dubourg,et al.Computed tomography angiography versus Agatston score for diagnosis of coronary artery disease in patients with stable chest pain: individual patient data meta-analysis of the international COME-CCT Consortium.DOI:10.1007/s00330-022-08619-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#AGA#
39
#PE#
39
#CTA#
50
#诊断价值#
36
#ATS#
60
#TST#
39