Lancet Oncol:PARP抑制剂Talazoparib在晚期转移性去势抵抗性前列腺癌中的抗肿瘤活性
2021-08-11 Nebula MedSci原创
Talazoparib在既往治疗过的携带DDR-HRR基因变异的晚期转移性去势抵抗性前列腺癌患者中有持久的抗肿瘤活性
PARP抑制剂在具有直接或间接参与同源重组修复(HRR)的基因DNA损伤反应(DDR)变异的转移性去势抵抗想前列腺癌中具有很好的抗肿瘤活性。
在TALAPRO-1研究中,研究人员评估了PARP抑制剂Talazoparib在携带DDR-HRR变异的转移性去势抵抗性前列腺癌中的活性和安全性。
TALAPRO-1是一项开放标签的2期试验,从多个国家的43家医院招募了年满18岁的、侵袭性、转移性、去势抵抗性前列腺腺癌患者,且要求携带已报道的对PARP抑制剂敏感的DDR-HRR基因变异(如ATM, ATR, BRCA1, BRCA2, CHEK2, FANCA, MLH1, MRE11A, NBN, PALB2, RAD51C),既往至少接受过一次针对转移的以紫杉烷为基础的化疗。受试患者接受Talazoparib口服(1 mg/天;中度肾损伤的患者0.75 mg/天),直到病情进展、出现不可耐受的毒性、调研员决定、撤出研究或死亡。主要终点是客观缓解率。
治疗反应
2017年10月18日-2020年3月20日,共招募了128位患者,其中127位至少接受了一剂Talazoparib治疗(安全性分析人群),104位有可测量的软组织病灶(抗肿瘤活性分析人群)。本次分析的截止日期为2020年9月4日。
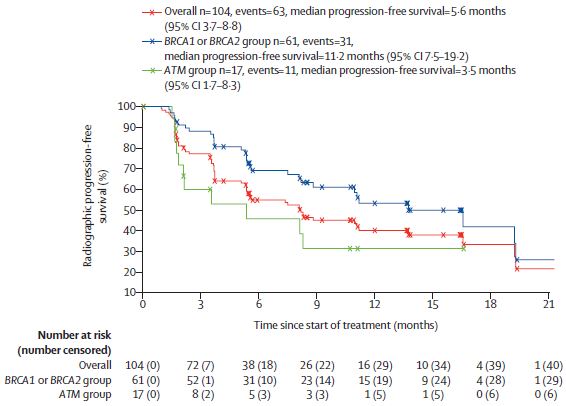
根据HRR基因变异分层的患者的无进展生存期
中位随访了16.4个月后,客观缓解率为29.8%。最常见的3-4级需紧急治疗的不良反应有贫血(31%)、血小板减少(9%)和中性粒细胞减少(8%)。43位(34%)患者报告了重度需紧急治疗的不良事件。无治疗相关死亡。
综上,Talazoparib在既往治疗过的携带DDR-HRR基因变异的晚期转移性去势抵抗性前列腺癌患者中有持久的抗肿瘤活性。该研究结果支持进一步开展更大规模的随机试验以验证Talazoparib在这类患者中的疗效。
原始出处:
Johann S de Bono, et al. Talazoparib monotherapy in metastatic castration-resistant prostate cancer with DNA repair alterations (TALAPRO-1): an open-label, phase 2 trial. Lancet Oncol. August 10, 2021. https://doi.org/10.1016/S1470-2045(21)00376-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















学习
44
#抗性#
64
#抑制剂#
38
#PARP抑制剂#
81
#肿瘤活性#
0
#抗肿瘤活性#
33
#Oncol#
31
#AZ#
33
挑好的
58
学习了,谢谢分享
52