原发性宫颈腺泡状软组织肉瘤 1 例
2020-06-26 张文哲 蒲盈盈 李丽 现代妇产科进展
患者, 23 岁, 3 年前曾因“无明显诱因出现经期延长、月 经量增多”于当地医院就诊。因否认性生活,未行妇科检查, 按“功能失调性子宫出血”给予雌孕激素、中药等治疗,效果 欠佳。
1 病例简介
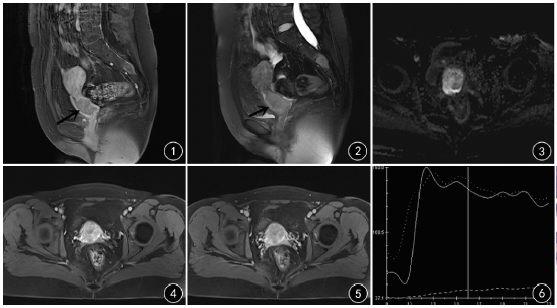
患者, 23 岁, 3 年前曾因“无明显诱因出现经期延长、月 经量增多”于当地医院就诊。因否认性生活,未行妇科检查, 按“功能失调性子宫出血”给予雌孕激素、中药等治疗,效果 欠佳。2016 年 3 月妇科检查示: 宫颈前唇可见一肿物凸起, 质硬,直径约 4cm,与宫颈周围组织分界不清,表面布满异型 增粗血管,蒂位于宫颈管内,后唇轮廓清,宫颈外口可见。遂 行“宫腔镜下宫颈肿物切除术+处女膜修补术”。术后病理 结果示:( 宫颈) 送检组织由弥漫性片状生长的肿瘤细胞构 成,瘤细胞体积大,界限清楚,圆形或多角形,胞质丰富、透明 或嗜酸性,空泡状核,核仁明显,不除外腺泡状软组织肉瘤。 为求进一步诊治,遂就诊于我院,病理科会诊示:( 宫颈前唇) 宫颈腺泡状软组织肉瘤。免疫组化: TFE-3( +) , PAS( +) , CK( -) , CD68( -) , CD34 血管( +) , Vimentin( -) , S-100( -) , Ki-67 阳性率<5%,见图 1。盆腔 MRI 示: 宫颈肿瘤术后改 变,未见肿瘤征象; 宫腔少量积血。上腹部 MRI 平扫、胸部 CT 平扫未见明显异常。肿瘤标记物未见异常。遂于 2016 年4 月行"腹腔镜下次广泛子宫切除术+双侧输卵管切除术+ 盆腔淋巴结清扫术"。术中探查见: 子宫前位,大小正常,形 态规则,双侧附件未见明显异常,盆腔各组淋巴结未见肿大。 术后病理:腺泡状软组织肉瘤; 子宫及双侧输卵管组织未查 见残余肿瘤;左髂总淋巴结 3 枚、右髂总淋巴结 5 枚、左盆腔 淋巴结 17 枚及右盆腔淋巴结 13 枚均未查见转移肿瘤。术 后未行放化疗。随访至 2019 年 5 月,术后 36 个月未见复发 及转移。
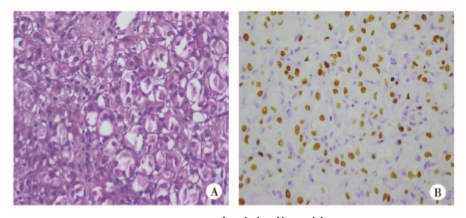
图 1 免疫组化图片 A:肿瘤细胞呈腺泡状排列,胞质丰富,内见嗜酸性细颗粒状 ( HE×400) ; B:肿瘤细胞 TFE3 呈细胞核弥漫着色( 免疫组化 染色×400)
2 讨 论
腺泡状软组织肉瘤( alveolar soft part sarcoma, ASPS) 是 一种罕见的组织来源不明的恶性软组织肿瘤,好发于肢体远 端,最常见部位是躯干和四肢,易发生早期转移,主要转移部 位是肺,其次是脑、骨和肝脏[1]。原发于宫颈的 ASPS 极其 罕见,目前国内外共有24 例报道。宫颈 ASPS 患者的年龄 8 ~68 岁,平均 31.2 岁。临床主要症状为不规则阴道流血,经 量增多,有的患者无明显症状,多于盆腔超声检查或行妇科 检查时发现宫颈肿物。宫颈 ASPS 多为结节状或片状,边界 尚清,部分肿瘤呈浸润性生长,肿瘤大小 0.2 ~ 8cm。宫颈 ASPS 质地较软,切面呈灰红、灰黄或灰褐色,鱼肉状。体积 较大的肿瘤常见出血、坏死灶及囊性变。光镜下: 典型的宫 颈 ASPS 肿瘤细胞排列成腺泡状或器官样结构。肿瘤细胞体 积大、多边形; 胞质丰富,内见嗜酸性细颗粒状,胞质内常可 见呈菱形或棒状结晶状包涵体, PAS 染色呈阳性;细胞核大, 异型性低( 最高为中度) ,有丝分裂不常见。根据特有的细胞 形态及细胞排列方式、细胞质内可见 PAS 包涵体及 TFE3 阳 性有助于 ASPS 的诊断和鉴别诊断。 宫颈 ASPS 早期难以明确诊断,易误诊,需依靠病理检查 明确诊断,免疫组化染色 TFE3 阳性有助于鉴别诊断。因宫 颈 ASPS 罕见,目前尚无统一的治疗方案。患者多行子宫切 除,包括子宫全切除术、广泛性子宫切除术、次广泛子宫切除 术,双附件是否切除可根据患者的年龄、生育要求等而定。 文献报道,放疗可作为术后辅助治疗,但不能提高生存率。 文献报道,术后随访时间 3~240 个月,平均 36.81 个月,随访 期间均未见复发及转移。本例患者于当地医院行肿瘤切除 术,术后未行放化疗,随访 36 个月未见肿瘤转移及复发。宫 颈 ASPS 的预后较其他常见部位的宫颈 ASPS 及常见宫颈恶 性肿瘤好,推测与该部位肿瘤生长缓慢、范围局限、不易发生 远处转移有关。
参考文献略。
原始出处:
张文哲,蒲盈盈,李 丽,张友忠等,原发性宫颈腺泡状软组织肉瘤 1 例报道并文献复习[J],现代妇产科进展,2020,29(6)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#原发性#
36
学习
97
了解一下
95
#宫颈#
23
#软组织#
39