Circulation:V因子Leiden与动脉血栓形成事件风险的相关性
2020-08-11 MedSci原创 MedSci原创
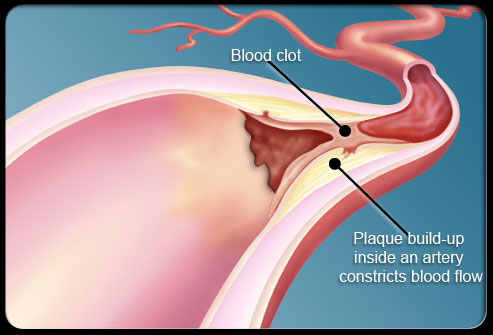
鉴于凝血参与动脉粥样硬化斑块破裂后的血栓形成阶段,研究人员推测V因子Leiden可能是冠心病(CHD)患者发生血栓形成事件的一个较强的危险因素。本研究旨在评估V因子与动脉血栓形成的相关性。
目前缺乏V因子Leiden在高动脉血栓形成风险患者中的作用的研究。鉴于凝血参与动脉粥样硬化斑块破裂后的血栓形成阶段,研究人员推测V因子Leiden可能是冠心病(CHD)患者发生血栓形成事件的一个较强的危险因素。
Mahmoodi等进行了一项个体水平的Meta分析,纳入了25个前瞻性研究(18个队列、3个病例队列、4个随机试验),共包含69681位受试者,其中3190位(4.6%)位V因子Leiden的杂合或纯合突变携带者。
中位随访1-10.6年。共20个研究的61147位受试者和6849例事件被纳入主要预后分析。V因子Leiden与心肌梗死和CHD死亡的复合预后无关(风险比[HR] 1.03,95% CI 0.92-1.16,p=0.12)。亚组分析未见相关差异。与此类似,次要预后(包括卒中、冠脉重建、心血管死亡和全因死亡率)的风险评估也几乎相同。
结论:在已确诊和治疗中的冠心病患者中,V因子Leiden与随后的动脉血栓形成事件和死亡率风险增加无关。
原始出处:
Bakhtawar K. Mahmoodi,et al. Association of Factor V Leiden With Subsequent Atherothrombotic Events. Circulation. 2020;142:546–555
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#动脉血#
55
#相关性#
31
#动脉血栓#
39
#动脉血栓形成#
42
#动脉血栓形成#
41
学习了
88
学习了
95
学习了
96