European Radiology:超快速动态增强乳腺MRI在乳腺癌新辅助治疗与病理完全缓解中的应用
2022-06-04 shaosai MedSci原创
乳腺超快DCE-MRI具有非常高的时间分辨率,扫描时间大约在4到7秒之间,并可在非常早期的时间点提供动力学信息。
现阶段,新辅助化疗(NAC)已成为局部晚期乳腺癌的标准治疗方法。试验表明,HER2阳性或三阴性乳腺癌患者在接受NAC治疗后有残余病变,转而接受特定的辅助治疗可演唱寿命,因此准确评估病理完全反应(pCR)的预后作用也变得越来越重要。
动态对比增强(DCE)MRI已被广泛用作评估NAC后乳腺癌肿瘤反应的成像方式,但由于成本和扫描时间问题,MRI的使用受到限制。乳腺超快DCE-MRI具有非常高的时间分辨率,扫描时间大约在4到7秒之间,并可在非常早期的时间点提供动力学信息。研究报告指出,与传统DCE-MRI的动力学曲线分析相比,这种早期动力学信息在区分乳腺良性病变和恶性病变方面具有相当的准确性,这意味着超快DCE-MRI的极早期阶段可以替代传统DCE-MRI的延迟阶段。然而据我们所知,还没有关于治疗前超快DCE-MRI得出的早期动力学参数与浸润性乳腺癌患者NAC后pCR之间关系的研究发表。
近日,发表在European Radiology杂志的一项研究探讨了超快速DCE- MRI的治疗前动力学特征与浸润性乳腺癌患者pCR之间的关系,并进一步评估其免疫组化(IHC)亚型的相关性,为乳腺癌患者的术前无创准确评估提供了技术支持。

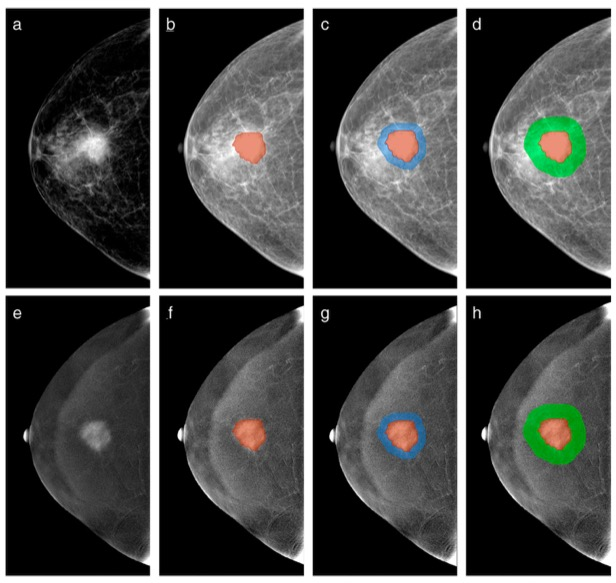
本研究于2018年8月至2019年6月纳入了256名连续的乳腺癌患者(平均年龄,50.2岁;范围,25-86岁),每位患者均在新辅助化疗后同时接受了超快、常规DCE-MRI和手术。DCE-MRI的动力学特征从治疗前的MRI数据中获得。增强时间、最大斜率(MS)以及U1和U2的体积(U1,病变开始增强的时间点;U2,U1后的后续时间点)来自于超快MRI。进行Logistic回归分析以确定与pCR相关的因素。
总的来说,所有患者中有41.4%达到了pCR。当包括所有乳腺癌时,没有一个动力学特征与pCR相关。在超快DCE-MRI动力学特征中,激素受体(HR)阳性乳腺癌中,较低的MS(OR,0.982;P = 0.040)与pCR相关。在三阴性乳腺癌中,较高的体积比U1/U2在单变量(OR, 11.787; p = 0.006)和多变量分析(OR, 14.811; p = 0.005)与pCR相关。在传统的DCE-MRI动力学特征中,在单变量分析中,较低的峰值增强(OR,0.993;p = 0.031)和较低的廓清百分比(OR,0.904;p = 0.039)仅与HR阳性乳腺癌的pCR有关。
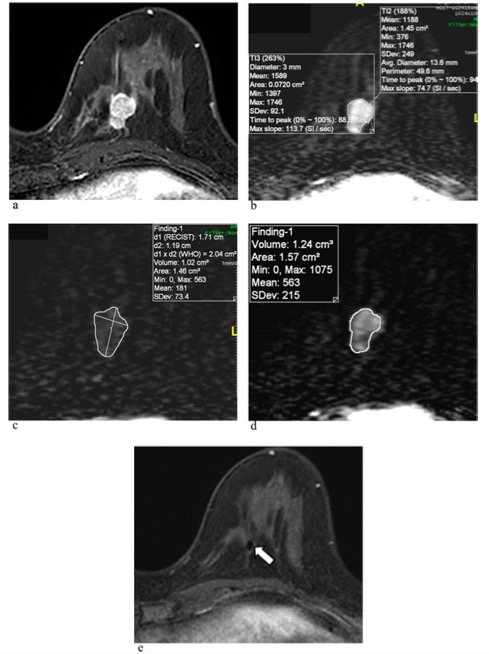
图 一位患有三阴性浸润性导管癌的52岁女性在接受NAC治疗后获得的pCR图像。a 治疗前早期增强MRI扫描显示左乳内上象限病变可见强化。b 在肿瘤最快速增强的部分放置一个3×3毫米的圆形ROI来计算最大斜率,同时在肿瘤的增强部分的超快速DCE-MRI上手动放置一个ROI。肿瘤体积是在U1(c)和U2(d)时间点用超快DCE-MRI测量的,U1/U2体积比为0.82。 e 治疗后的早期增强MRI扫描显示夹子标记周围没有残留的增强,该标记以前曾被插入肿瘤内(箭头)
本研究发现,超快DCE-MRI特征与浸润性乳腺癌的pCR相关,但具体特征根据IHC亚型而不同。在三阴性浸润性乳腺癌中,来自超快DCE-MRI的U1/U2的较高体积比与pCR独立相关。
原文出处:
Ji Hee Kim,Vivian Youngjean Park,Hye Jung Shin,et al.Ultrafast dynamic contrast-enhanced breast MRI: association with pathologic complete response in neoadjuvant treatment of breast cancer.DOI:10.1007/s00330-021-08530-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#病理完全缓解#
58
#新辅助#
46
#PE#
51
#完全缓解#
45
#学习##期刊论坛#
61
不错的文章
33