Nat Neurosci:研究揭示压力可影响乳腺癌病情,神经疗法或有抑制效果
2019-07-18 佚名 中国生物技术网
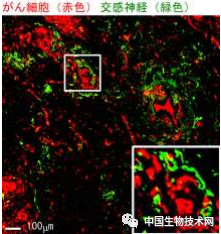
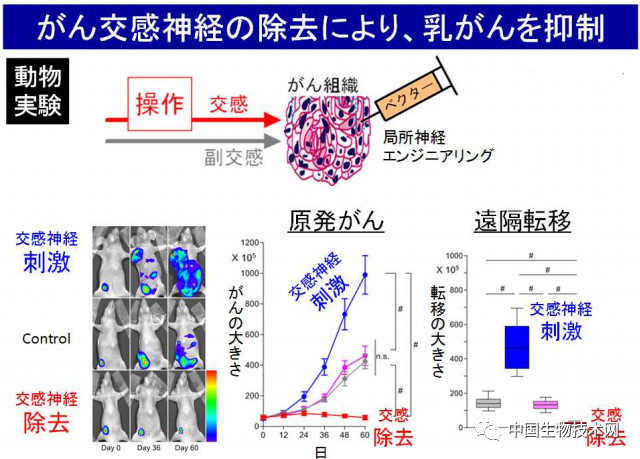
日本冈山大学和日本国立癌症研究中心等机构9日宣布,他们开展的一项最新研究发现,压力等因素导致的交感神经兴奋会影响乳腺癌的病情进展。这表明神经疗法有可能成为新的癌症治疗方法。该研究7月8日已发表在《Nature Neuroscience》上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
32
#病情#
35
#ROS#
40
好
87
学习了
100
学习谢谢分享
92
学习了,谢谢分享
88
好好好好好好
84
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
34