罕见病例:一例特殊的异位妊娠
2018-04-04 MedSci MedSci原创
这是去年的一份病例。患者是由急诊转上来的,平车推入,侧身捂着下腹。当时,患者面色苍白,神情痛苦,询问病情也只是哼哼着说肚子疼。转移到检查室上后,我让她保持平卧,按压了一下她的腹部,右下腹有明显压痛反跳痛。腹部叩诊发现移动性浊音可疑。 妇科专科检查:外阴发育正常,已婚未产式,阴道畅,正常分泌物,宫颈质中,常大,子宫前位,常大,质中,漂浮感,双附件区增厚,压痛(腹壁对抗)。后穹窿稍饱满,触痛,以右侧
这是去年的一份病例。患者是由急诊转上来的,平车推入,侧身捂着下腹。当时,患者面色苍白,神情痛苦,询问病情也只是哼哼着说肚子疼。转移到检查室上后,我让她保持平卧,按压了一下她的腹部,右下腹有明显压痛反跳痛。腹部叩诊发现移动性浊音可疑。
妇科专科检查:外阴发育正常,已婚未产式,阴道畅,正常分泌物,宫颈质中,常大,子宫前位,常大,质中,漂浮感,双附件区增厚,压痛(腹壁对抗)。后穹窿稍饱满,触痛,以右侧为甚。患者的血压偏低,而且心率较快。根据平常经验,很有可能是异位妊娠,而且已经出现破裂的情况。
虽然基本已经明确诊断,但仍需完善检查,做好术前准备。
经阴道超声检查显示右附件包块4cmX4cm大小。
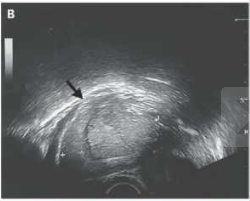
同时发现了腹腔游离液体,但是宫内这个囊泡是什么情况呢?

通过超声,这明显是一例比较少见的妇产科疾病。为了更好地确定诊断,进行了腹部超声检查。结合患者腹部超声影像可以明确这是一例宫内外复合妊娠的病例。

在逐在完善相关检查及手续后,对患者实行了急诊腹腔镜手术,腹腔镜下,可见一个完整的妊娠囊、胚胎和右输卵管破裂。由于破裂的输卵管大量出血导致腹腔内大量积血。最后对其进行输卵管切除术。

在切除右输卵管后,患者恢复良好,预后较佳,继续宫内妊娠,足月后产下一个健康的女孩。
一家人幸福美满,未来阳光灿烂。
简析:
复合妊娠(heterotopicpregnancy,HP)指同时发生在2个或以上种植部位的妊娠,包括宫内外复合妊娠、双侧输卵管同时妊娠、输卵管合并卵巢妊娠等,其中以宫内外复合妊娠最常见。国内外许多文献中将“heterotopic pregnancy”等同于宫内外复合妊娠,这种理解是不全面的。宫内外复合妊娠在自然妊娠中非常罕见,发生率约1/30 000,随着辅助生殖技术广泛开展,其发生率明显增高,达1%左右。笔者所在医院1 476例体外受精-胚胎移植(IVF-ET)后妊娠中发生12例(0.81%)宫内外复合妊娠。肖红梅等对2322例IVF-ET后妊娠进行分析,异位妊娠发生率为4.05%(94/2322),其中宫内外复合妊娠发生率为0.86% (20/2322)。
宫内外复合妊娠中最常见类型为宫内合并输卵管妊娠,约占88.2%,少见类型包括宫内妊娠合并宫角妊娠、宫颈妊娠、子宫瘢痕妊娠、卵巢妊娠、残角子宫妊娠、腹腔妊娠等。
宫内外复合妊娠临床表现无特异性,主要表现为腹痛及阴道流血。超声是宫内外复合妊娠的主要诊断方法,多数在孕早期得到诊断。文献报道,在辅助生殖后未破裂和已破裂的宫内外复合妊娠中,分别有66.7% 和85.7% 的病例在妊娠7周前通过超声诊断。由于自然妊娠后的宫内外复合妊娠病例少,尚未见相关数据总结。Soriano等比较了腹腔镜确诊的12例宫内外复合妊娠和210例异位妊娠,发现两组在腹痛、阴道流血的发生率及类型差异无统计学意义。4例(33.4%)宫内外复合妊娠和29例(13.8%)异位妊娠患者出现失血性休克,需要输血。
宫内外复合妊娠易于漏诊,主要原因包括对宫内外复合妊娠的警惕性不足,超声发现宫内妊娠存在的证据,使超声医生或妇产科医生认为能够同时排除异位妊娠的存在,以及宫内外复合妊娠缺乏特异性的症状和体征。一项对82例宫内外复合妊娠进行回顾的文献报道显示,有33%复合妊娠在第1次超声检查时漏诊,仅发现1个或多个宫内妊娠。当然,不能完全排除异位妊娠生长速度慢于宫内妊娠,导致超声诊断困难。在临床工作中,若出现以下情况需要警惕宫内外复合妊娠的存在:(1)辅助生殖技术后妊娠。(2)在人工流产、自然流产进行诊刮后hCG持续不降或升高。(3)子宫明显大于停经天数。(4)在自然妊娠后出现不止1个黄体。(5)在异位妊娠的症状和体征明确存在时,无阴道流血。
宫内外复合妊娠治疗方式的选择首要取决于宫内妊娠情况以及患者保留宫内妊娠的意愿。若宫内妊娠发育不良或不需要保留宫内妊娠,则复合的异位妊娠的治疗方式无异于一般的异位妊娠。若宫内妊娠发育正常,且患者需要保留,则宫外妊娠治疗方案的选择取决于异位妊娠的部位、异位妊娠包块大小、是否破裂出血、hCG值、患者生命体征是否平稳等,包括期待治疗、保守治疗、手术治疗以及少见的治疗方式。当异位妊娠位于宫颈、子宫瘢痕处、宫角等部位时,与宫腔关系密切,治疗时需要特别考虑对宫内妊娠的影响。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#罕见病例#
0
学习
82
涨姿势了
72
#异位妊娠#
46
#罕见#
58
学习学习学习
88
宫外复合妊娠确实是少见!
84