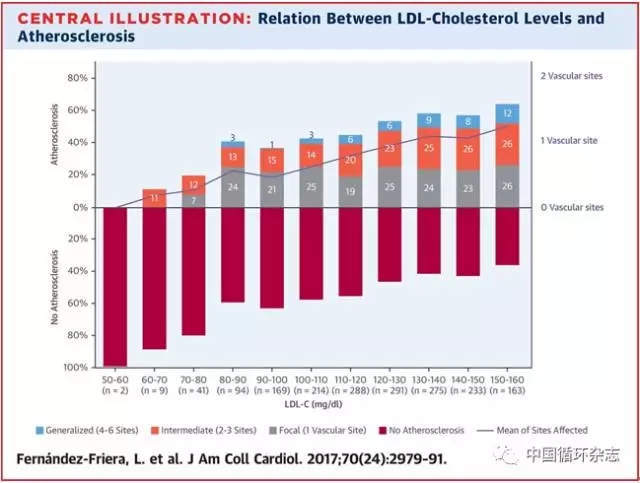
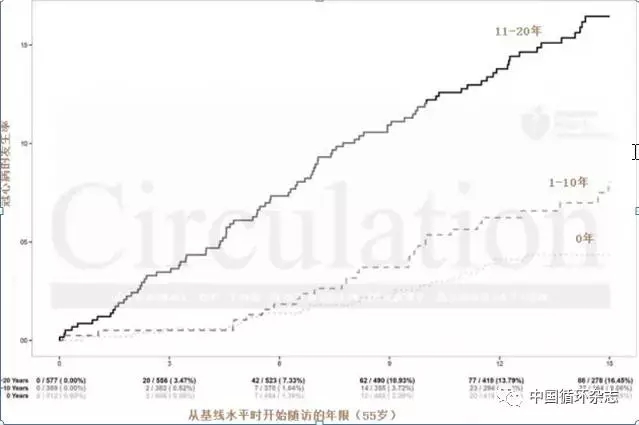
JACC:半数中年人有动脉粥样硬化,控制坏胆固醇还应加强?
2017-12-14 卢芳 中国循环杂志
近期一项发表在JACC的研究显示,中年人群,纵使不胖不瘦,不吸烟,也没有“三高”,但还是挡不住岁月的洗礼——近半人有动脉粥样硬化斑块。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#粥样硬化#
31
#JACC#
28
#ACC#
30
#中年人#
23
学习了受益匪浅
62