Science Signaling:北京大学王韵团队揭示催产素相关信号可能是治疗自闭症的关键
2022-02-03 “生物世界”公众号 “生物世界”公众号
社交记忆允许个体将朋友和默生者区分开来,并适当缇欧着你自己的行为,这对于合作和交配等亲社会行为至关重要,是动物的一种基础社交行为,对于人类也是也同样如此。
社交记忆允许个体将朋友和默生者区分开来,并适当缇欧着你自己的行为,这对于合作和交配等亲社会行为至关重要,是动物的一种基础社交行为,对于人类也是也同样如此。
自闭症谱系障碍和精神分裂症等疾病均伴有社交行为异常,并可能表现出社交记忆的损伤。催产素受体(Oxytocin receptor,OXTR)是社交相关行为在分子水平调控的研究重点,也是相关疾病的治疗靶点。OXTR属G蛋白偶联受体(GPCR),此前的研究发现其第三胞内环C端存在多个潜在的磷酸化修饰位点,但其功能研究仅局限于分子水平,尚未阐明OXTR的翻译后修饰与特异脑区功能或社交行为的联系。
2022年2月1日,北京大学医学部神经科学研究所、北京大学IDG-麦戈文脑科学研究所王韵教授课题组在 Science 子刊 Science Signaling 发表了题为:Phosphorylation-dependent positive feedback on the oxytocin receptor through the kinase PKD1 contributes to long-term social memory 的研究论文。
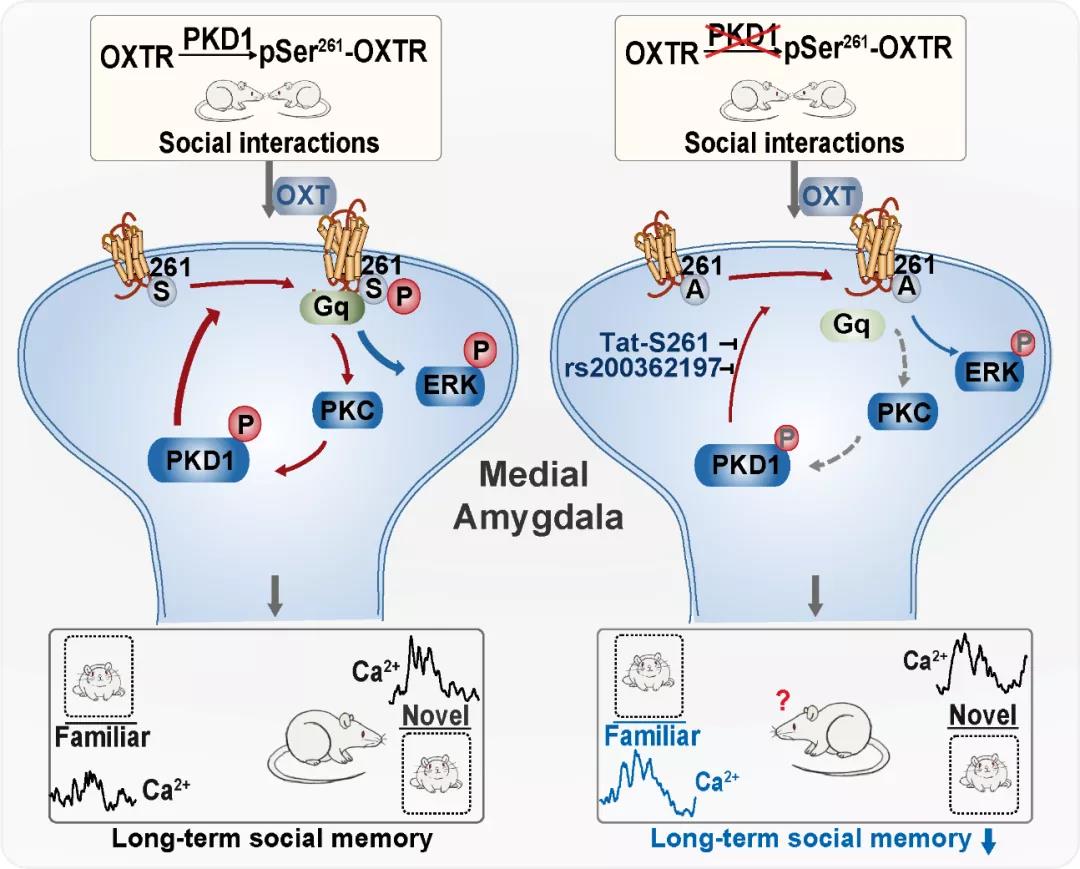
该研究发现社交记忆依赖于“爱情激素”催产素相关的信号通路,并进一步揭示了蛋白激酶D1(Protein kinase D1,PKD1)与催产素受体(Oxytocin receptor,OXTR)的相互磷酸化特异性调控内侧杏仁核(Medial amygdala,MeA)介导的长时程社交记忆及其潜在机制。

PKD是一类新发现的在进化上高度保守的丝苏氨酸蛋白激酶,属于钙调蛋白激酶超家族(CaMKs)。在哺乳动物中,PKD包含三个亚型:PKD1、PKD2和PKD3,在肺和大脑组织中有较高的表达量。其中,PKD1作为细胞内多种信号通路的关键节点,参与多种生物学功能如细胞的增殖和分化、囊泡的运输和分泌、免疫调节以及心肌的舒张和收缩,对细胞骨架、信号分子和离子通道等存在多重调控。
王韵课题组自2003年开始探讨PKD1及其下游底物在神经系统功能调控及分子机制,首次报道了PKD1在神经系统的功能,发现在外周伤害性感受器背根神经节中PKD1可通过磷酸化辣椒素受体,也称为瞬时感受器受体潜在的阳离子亚家族V1成员(TRPV1)在痛觉调控中发挥重要作用,随后发现PKD1在神经元的发育和迁移,突触发生,突触可塑性,学习记忆以及药物成瘾中发挥了至关重要的作用。
而该研究首次发现,PKD1可以磷酸化催产素受体OXTR第261位丝氨酸(S261),将OXTR S261突变为丙氨酸(S261A)使其无法磷酸化,导致下游的ERK1/2磷酸化水平降低,抑制MAPK通路活性。同时,PKD1与OXTR的相互作用特异性调控动物内侧杏仁核(Medial amygdala,MeA)脑区介导的长时程社交记忆。
通过催产素受体S261A基因敲入、MeA注射干扰肽Tat-S261等手段干扰OXTR S261的磷酸化,导致MeA介导的长时程社交记忆下降。而如果将OXTR S261突变为谷氨酸(S261E)模拟持续磷酸化状态,过表达在MeA脑区,可以部分挽救S261A基因敲入大鼠的长时程社交记忆受损。
进一步,通过将在体光纤记录(Fibre photometry)获取的实时钙信号与动物行为偶联,发现野生型大鼠MeA脑区的钙信号强度在面对陌生鼠时显着高于熟悉鼠,而催产素受体S261位丝氨酸突变的大鼠没有显着差异。进一步的研究显示,干扰OXTR第261位丝氨酸的磷酸化影响其与Gq/11蛋白之间相互作用,而OXTR的激活能够通过蛋白激酶C(Protein kinase C,PKC)依赖的途径提高PKD1的磷酸化水平,表明OXTR与PKD1存在相互作用的正反馈调控,从而实现催产素系统的信号放大。此外,OXTR中存在大量单核苷酸多态性(SNP)位点与焦虑、自闭症谱系障碍或精神分裂症等疾病具有很强的相关性。
研究发现第258位精氨酸发生突变的rs200362197会干扰PKD1对OXTR S261的磷酸化,提示携带SNP rs200362197可能导致异常的社交记忆能力。
总的来说,本研究首次阐述了催产素受体的磷酸化修饰在分子、脑区以及社交行为中多层次的调控作用,为OXTR的社交相关调控功能提供了位点及脑区特异性证据,同时为理解社交缺陷的分子机制提供了新的启示。
北京大学医学部神经科学研究所博士生王菲、尹湘莎是这篇论文的并列第一作者,北京大学医学部神经科学研究所、北京大学IDG麦戈文脑科学研究所王韵教授和岑程助理研究员是该论文的通讯作者。
原始出处:
FEI WANG, et al. Phosphorylation-dependent positive feedback on the oxytocin receptor through the kinase PKD1 contributes to long-term social memory. SCIENCE SIGNALING, 1 Feb 2022 ? Vol 15, Issue 719.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#signaling#
52
#Signal#
42
#北京大学#
56
值得研究
58
#Sign#
36
新发现,新知识
56
#SCIE#
36
#自闭#
37
#催产#
38