1、小结节影 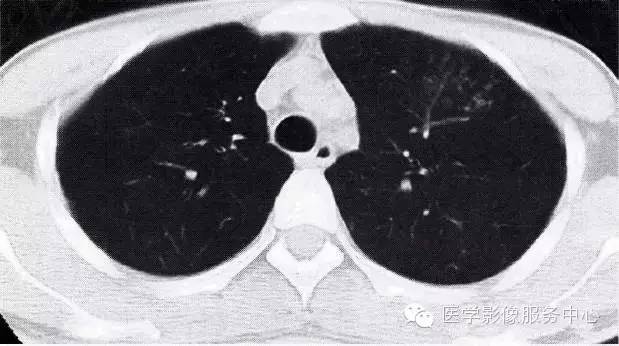
图1肺炎小结节影
2、小斑片状或斑片状的融合影
可见各种原因的肺炎。直径为1.0~2.5cm.边缘模糊。斑片影并可见发生融合,一般表现为:下比上多,内比外多,后比前多(图2)。
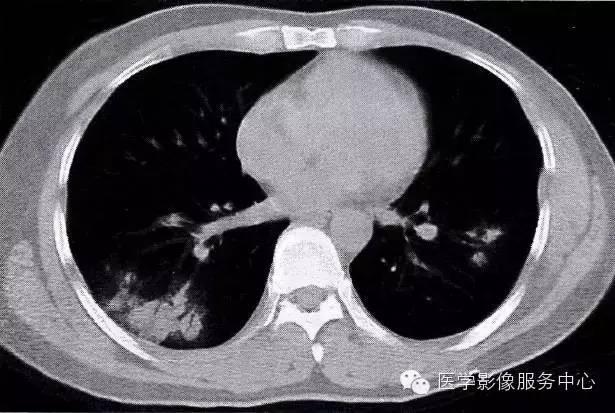
图2肺炎小斑片状影
双下肺小斑片状影肺炎,内有小的支气管影,斑片状影边缘模糊
3、肺段及大叶阴影
多见于细菌感染,也可见于腺病毒和卡氏囊虫感染。以肺段或叶为界的大片实变,体积不缩小,内有支气管充气征,边缘常较淡,模糊(图3)。

图3肺炎大片状实变
左肺上叶大片状实变影,体积不缩小,其内有支气管空气征
4、条索状及网状阴影
此征常见于放射性肺炎,慢性肺炎,间质性肺炎和肺炎的吸收期。病变为增殖为主,也可合并有实质性肺泡炎。表现为斑片状不规则的条索状混合影。边缘可清楚,也可模糊(图4,图5)。
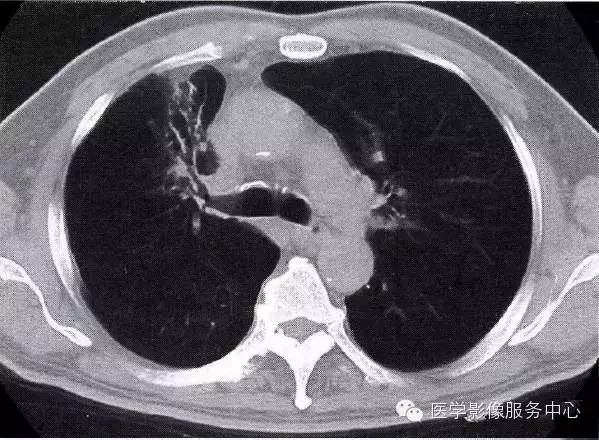
图4慢性肺炎条索状影
右肺上叶前段条索状影,内有小的支气管扩张

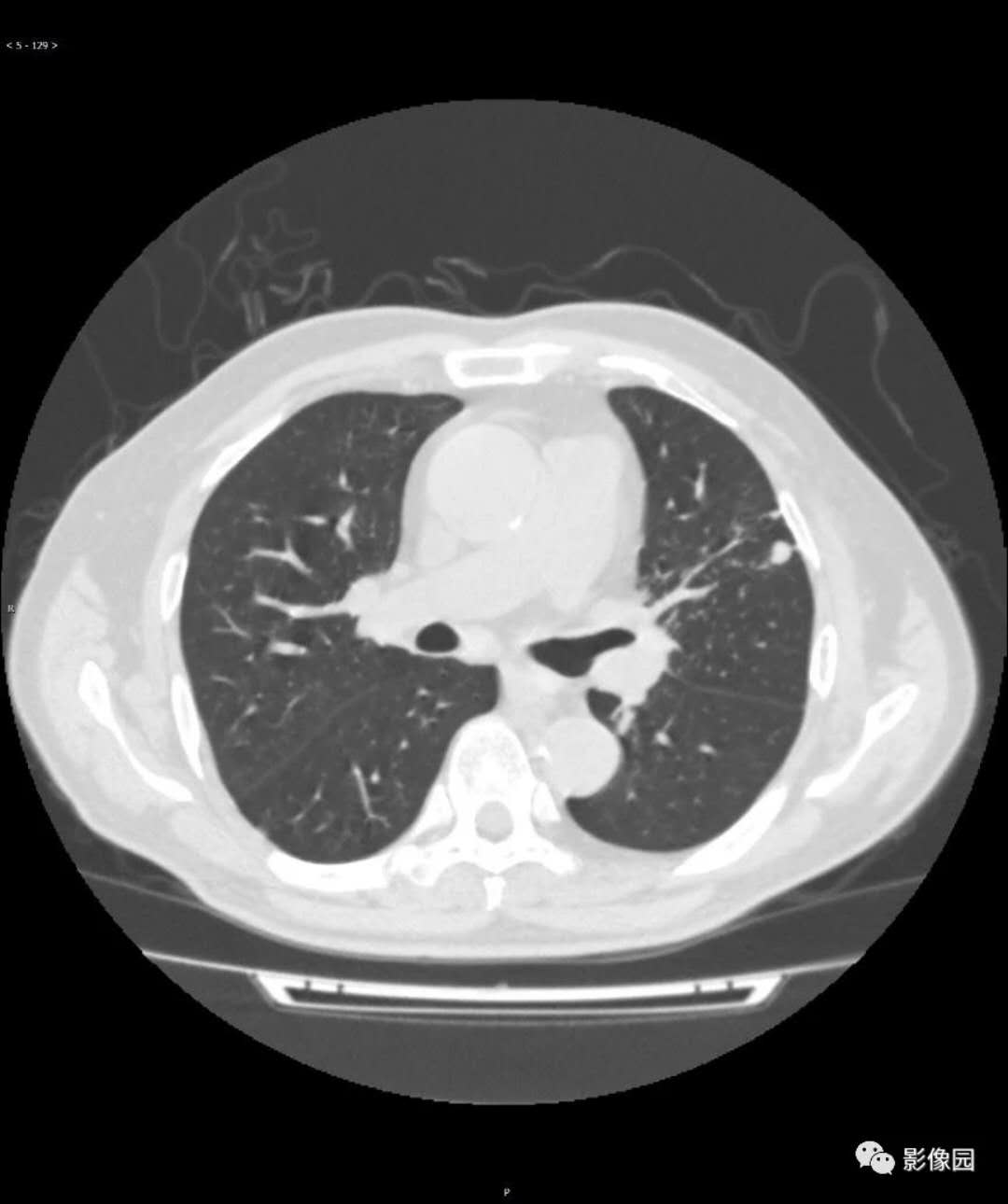
图5肺炎吸收期
双肺多发条索影及网格状影
5、球形阴影

图6球形肺炎
右肺上叶尖段可见一球形结节状影,边缘模糊

图7球形肺炎
与图2-6为同一患者,经抗感染治疗后2周,病灶明显缩小

图8右肺上叶脓肿伴空洞
脓肿空洞为厚壁,内壁不规则,周围有斑片状影,边缘模糊
7、胸膜病变
合并积液,后期胸膜局部增厚。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#肺部炎症#
50
谢谢分享
67
#CT表现#
49
感谢提供这么好的东西
64
写的太不详细了
90
学习了
63
可以
61
讲的很实用,谢谢分享
72