Lancet:Ziltivekimab可有效降低高动脉粥样硬化风险个体的炎症标志物
2021-05-19 Nebula MedSci原创
采用Ziltivekimab抑制IL-6明显减少了与动脉粥样硬化相关的炎症和血栓形成的生物标志物
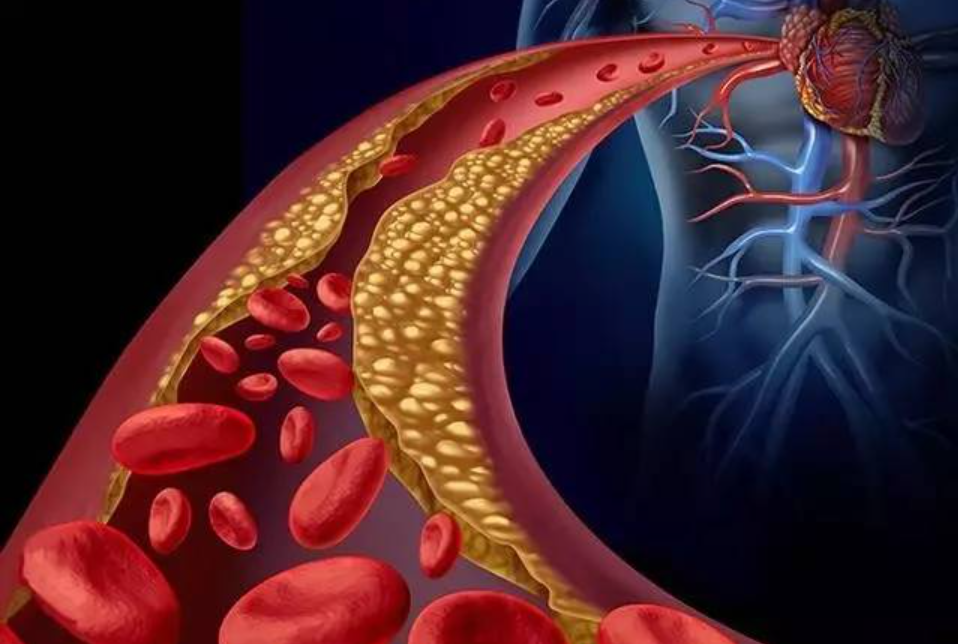
IL-6已成为动脉粥样硬化血栓形成的关键因素。但IL-6抑制在高动脉粥样硬化风险但无系统炎症疾病的个体中的安全性和有效性尚不清楚。

Ziltivekimab是一种靶向IL-6配体的一种纯人单克隆抗体。Ridker等人探讨了Ziltivekimab用于高心血管风险的患者降低炎症和血栓生物标志物的有效性和安全性。
RESCUE试验是一项在美国的40个医疗地点开展的随机双盲的2期研究,招募了年满18岁的、有高敏感性C反应蛋白(CRP)升高(>2mg/l)的中重度慢性肾病患者。按1:1:1:1将受试者随机分至4组,分别接受安慰剂或Ziltivekimab 7.5 mg、15 mg或30 mg,1次/4周,持续24周。主要终点是高敏感性CRP的变化。
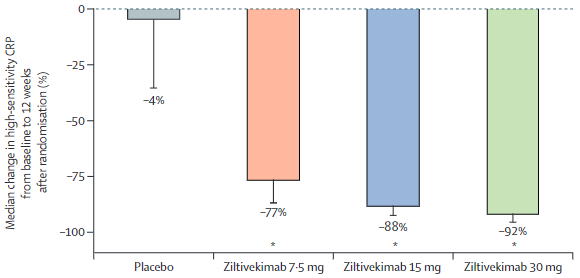
随机化分组后12周时CRP的变化
2019年6月17日-2020年1月14日,共招募了264位患者,每组分了66位患者。在随机化分组后12周时,7.5 mg组、15 mg组、30 mg组和安慰剂组的中位高敏感性CRP水平分别降低了77%、88%、92%和4%。
因此,根据分层校正后,Ziltivekimab和安慰剂组之间高敏感性CRP百分比变化的对比差异为:7.5 mg组 -66.2%;15 mg组 -77.7%;30 mg组 -87.8%(所有p<0.0001)。
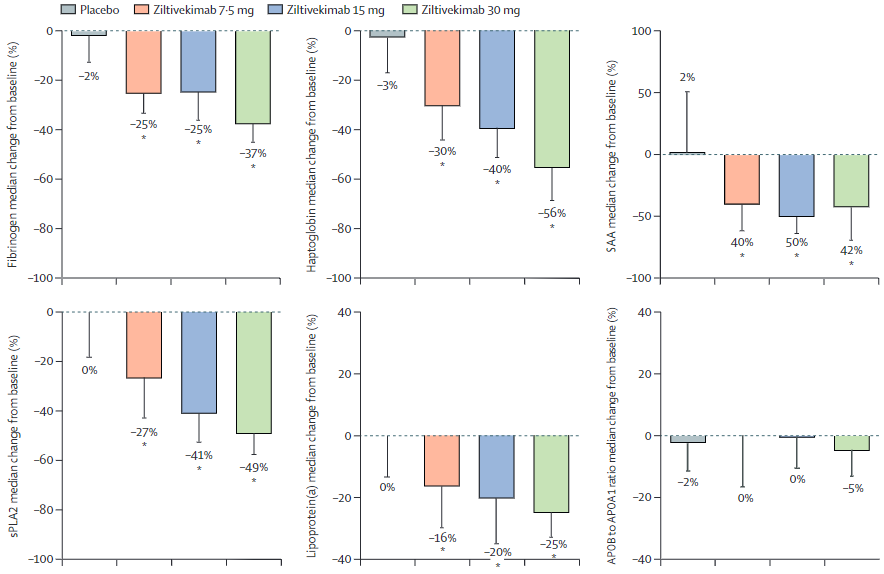
纤维蛋白原、血清淀粉样蛋白A、触珠蛋白、分泌型磷脂酶A2和脂蛋白(a)的变化
在24周的治疗期内效果稳定。此外,纤维蛋白原、血清淀粉样蛋白A、触珠蛋白、分泌型磷脂酶A2和脂蛋白(a)也呈现出剂量依赖性的降低。
Ziltivekimab的耐受性良好,不影响总胆固醇与高密度脂蛋白胆固醇的比例,也没有严重的注射部位反应、持续的3级或4级中性粒细胞减少症或血小板减少症。
不良反应
总之,Ziltivekimab明显减少了与动脉粥样硬化相关的炎症和血栓形成的生物标志物。基于这些数据,一项大规模的心血管预后试验将评估Ziltivekimab在慢性肾脏疾病、高敏性CRP升高的已确诊的心血管疾病患者中的作用。
原始出处:
Paul M Ridker, et al. IL-6 inhibition with ziltivekimab in patients at high atherosclerotic risk (RESCUE): a double-blind, randomised, placebo-controlled, phase 2 trial. The Lancet. May 17, 2021. https://doi.org/10.1016/S0140-6736(21)00520-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Lancet#
39
#mAb#
43
#粥样硬化#
38
#炎症标志物#
48
#标志物#
39
顶刊就是不一样,质量很高,内容精彩!学到很多
58
好
71