J Intern Med:新型胶原因子Endotrophin可预测动脉粥样硬化患者的心血管事件和死亡风险
2021-05-06 Nebula MedSci原创
PRO‐C6存在于动脉粥样硬化斑块中,并与患者未来的心血管事件、心血管死亡和全因死亡风险相关
动脉粥样硬化斑块破裂是急性心血管事件的主要原因。Endotrophin是一种VI型胶原因子,可采用生物标记物PRO-C6检测,或可为检测需要加强二级预防的心血管疾病患者提供有价值的信息。
本研究旨在通过检测动脉粥样硬化患者动脉粥样硬化斑块中的内啡肽和循环中的PRO-C6水平,以确定该生物标志物的在动脉粥样硬化患者中的预测价值。
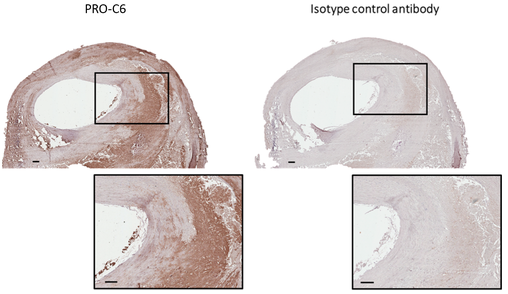
颈动脉斑块PRO-C6抗体染色
取人颈动脉斑块切片,进行PRO-C6抗体染色。检测了参加颈动脉斑块成像项目(CPIP)(发现队列,n=577)和IMI-Summit项目(验证队列,n=1378)的患者的血清PRO-C6水平。
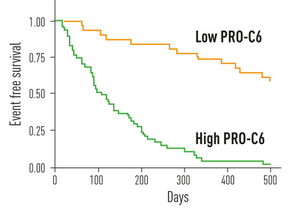
血清PRO-C6水平与患者无事件存活率的相关性
中位随访时间为43个月。PRO-C6定位于动脉粥样硬化斑块的核心和前部。在发现队列中, PRO‐C6可独立预测患者未来的心血管事件(HR 1.089 [95%CI 1.019-1.164],P=0.01)、心血管死亡(HR 1.118 [95%CI 1.008-1.241],P=0.04)和全因死亡(HR 1.087[95%CI 1.008-1.172],P=0.03)风险。
在验证队列中,验证了PRO‐C6可预测患者未来的心血管事件(OR 1.063 [95%CI 1.011-1.117],p=0.017)。
综上,在两个较大的前瞻性队列中,PRO‐C6存在于动脉粥样硬化斑块中,并与患者未来的心血管事件、心血管死亡和全因死亡风险相关,提示新型胶原因子Endotrophin可预测动脉粥样硬化患者的心血管事件和死亡风险。
原始出处:
Holm Nielsen S,Edsfeldt A,Tengryd C et al. The novel collagen matrikine, endotrophin, is associated with mortality and cardiovascular events in patients with atherosclerosis. J Intern Med, 2021, https://doi.org/10.1111/joim.13253
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#血管事件#
40
#Endotrophin#
64
#粥样硬化#
49
#死亡风险#
41
#Med#
44
#OTR#
24