Eur J Cancer: 卡博替尼(Cabozantinib)治疗转移性肾细胞癌的疗效:来自真实世界研究CABOREAL结果分析
2021-10-23 yd2015 MedSci原创
该最大型真实世界数据表明,卡博替尼(Cabozantinib)对未经选择既往治疗的转移性肾细胞癌患者有效。并且初始足剂量(60 mg/day)使用更能改善患者预后。
肾细胞癌(RCC)是最常见的肾癌,占所有成年男性恶性肿瘤的5%,女性恶性肿瘤的3%,约占所有肾癌的80%。许多肾细胞癌患者直到疾病晚期时仍无症状,其中25-30%的患者在诊断时出现转移。晚期肾细胞癌(aRCC)和转移性肾细胞癌(mRCC)患者5年生存率分别为45-65%和0-10%。卡博替尼(Cabozantinib)是一种口服的多酪氨酸激酶受体(TKIs)小分子抑制剂(包括MET, AXL, VEGFR-2)。在aRCC (METEOR)患者中开展的开放标签III期研究,评估cabozantinib在疾病进展后的有效性和安全性。研究表明,与依维莫司相比,cabozantinib显著延长了中位无进展生存期(PFS)(7.4个月vs 3.9个月,HR: 0.51[95%CI: 0.41-0.62], p <0.0001)和显著改善患者的中位总生存期(OS)(分别为21.4个月和16.5个月,HR: 0.66 [95% CI: 0.53-0.83],p = 0.00026)。来自法国的学者开展回顾性研究CABOREAL (NCT03744585),评估真实世界中卡博替尼(Cabozantinib)治疗转移性肾细胞癌(mRCC)的疗效。相关研究结果发表在European Journal of Cancer杂志上。
这项多中心(n=26)、观察性、回顾性研究纳入了接受≥1剂量cabozantinib的mRCC患者。使用kaplan meier法估算总生存期(OS);使用log-rank检验对亚组进行比较。多Cox回归模型评估卡博替尼治疗后OS的预测因素。
共有410例mRCC患者(男性74%,女性26%)被纳入研究。总的来说,mRCC的一线、二线和三线治疗的中位持续时间(四分位数[Q] 1-Q3)分别为9.1 (4.2-19.5)、5.6 (2.8-11.4)和5.3 (3.1-11.0)个月。总体而言,一半的患者(50.1%)既往接受过纳武利尤单抗治疗。mCRC诊断后到开始Cabozantinib治疗中位时间(Q1-Q3)为32.1 (17.4-56.6)个月。Cabozantinib的初始剂量为60mg (70.9%), 40mg(26.7%)和20mg(2.0%)。总体而言,cabozantinib中位(Q1-Q3)治疗持续时间为7.6 (3.2e15.7)个月。12个月时仍接受cabozantinib治疗的患者比例为34.9%。
半数以上的患者(57.0%)需要减少剂量。大多数患者(65.3%)暂时中断了1次cabozantinib治疗,中位数(Q1-Q3)为22.0 (12.5-51.0)天。不良事件(AE)是剂量调整和治疗中断的主要原因(92.5%和85.0%的患者因AE而调整/中断)。
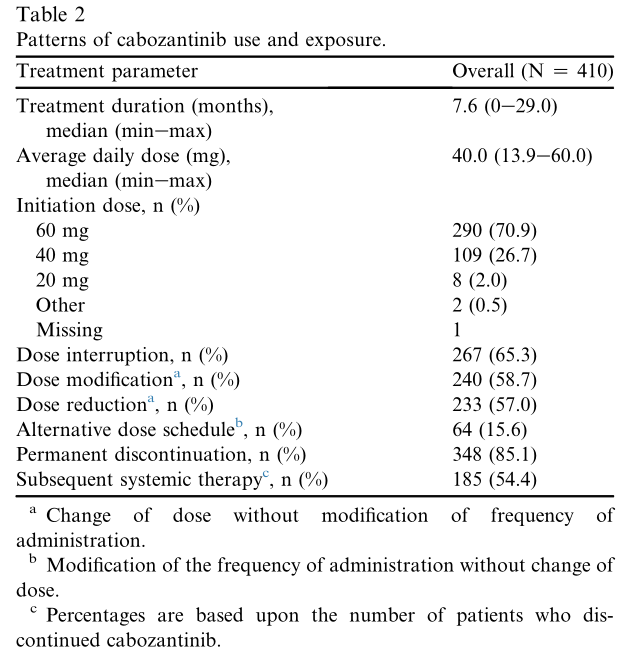
卡博替尼治疗剂量模式
随访期结束时,大多数患者(85.1%)永久停用了cabozantinib治疗,主要原因是疾病进展(54.9%)或出现AE(24.9%)。大约一半的患者(54.4%)继续接受后续的全身抗肿瘤治疗,主要是纳武利尤单抗(47.8%)、阿昔替尼(21.7%)和依维莫司(19.0%)。
总中位随访时间为14.4 (0-30)个月,其中67.1%的患者(275/410)死亡。死亡的主要原因为疾病进展(80.0%)。12个月时的OS率为56.5% (95% CI: 51.5-61.2),中位OS为14.4个月(95% CI: 12.4-16.2)。
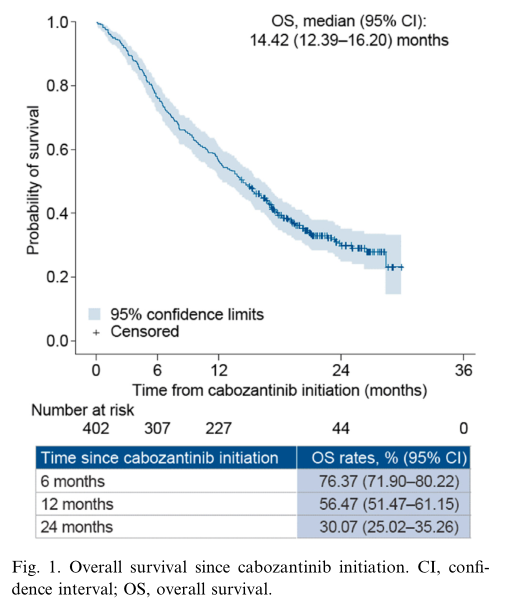
OS
老年患者(>75岁)的中位OS与年轻患者无显著差异(13.3个月vs 14.6个月,p=0.3200)。IMDC低风险和中度风险组比IMDC不良风险组的中位OS更长(未达到,17.8个月 vs 7.3个月)。同样,MSKCC低风险和中度风险组比MSKCC不良风险组的中位OS更长(未达到,20.2个月 vs 7.5个月)。骨和肝转移患者的中位OS为11.0个月,而无骨转移患者的中位OS为15.1个月(p=0.1413)。脑转移患者的中位OS明显短于无脑转移患者(11.3个月vs 15.5个月,p=0.0066)。与其他患者相比,使用过nivolumab的患者使用cabozantinib的治疗持续时间更长(9.3个月vs 6.2个月,p=0.0008)。初始剂量为60mg的患者中位OS较长(15.4个月vs 11.8个月,p=0.0314)。剂量减少的患者中位OS也更长(17.5个月vs 8.9个月,p<0.0001)。
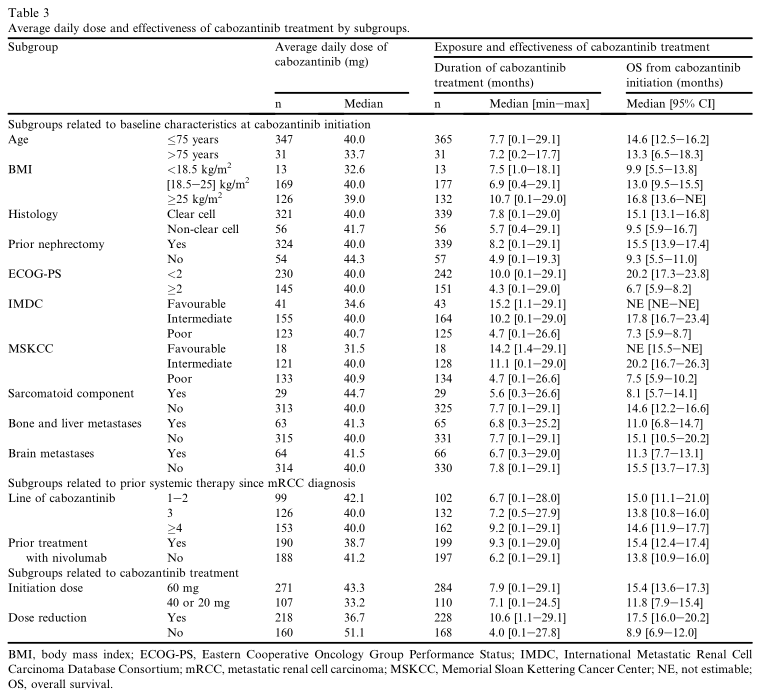
OS亚组分析
多变量分析显示,较长的生存时间与以下因素有关:体重指数(BMI)≥ 25kg /m2(与BMI 18.5-25kg / m2相比,HR =0.64;95% CI: 0.48-0.85, p=0.0021);既往肾切除术(HR=0.64;95% CI: 0.45-0.90, p=0.0109);和IMDC低风险(HR=0.15;95% CI: 0.08-0.29, p<0.0001)或IMDC中度风险(HR=0.38;95%CI:0.28-0.53, p<0.0001)与IMDC不良风险比较。较短的生存期与开始治疗未服用足剂量的cabozantinib相关(40/20 mg vs 60 mg, HR=1.35;95% CI: 1.00-1.82, p=0.0486)。
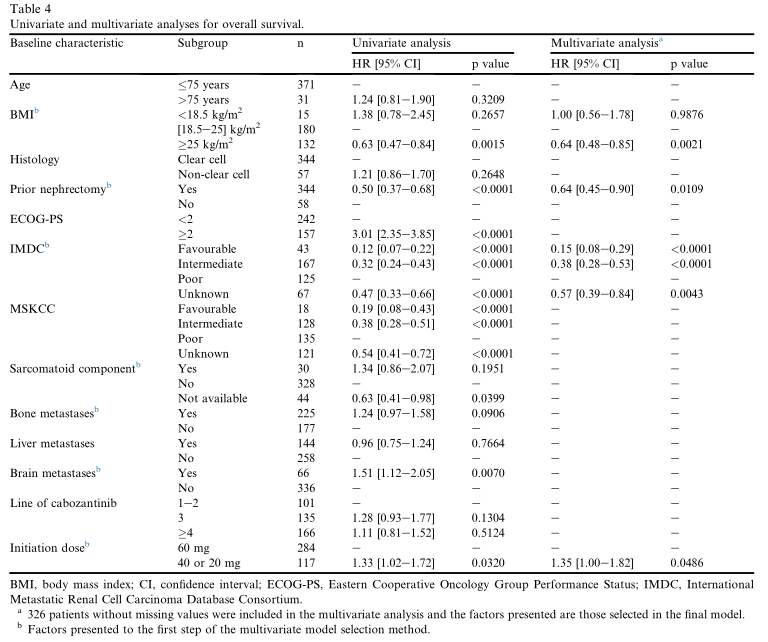
多变量分析
综上,该最大型真实世界数据表明,卡博替尼(Cabozantinib)对未经选择既往治疗的转移性肾细胞癌患者有效。并且初始足剂量(60 mg/day)使用更能改善患者预后。
原始出处:
Albiges L, Fléchon A, Chevreau C, Topart D, Gravis G, Oudard S, Tourani JM, Geoffrois L, Meriaux E, Thiery-Vuillemin A, Barthélémy P, Ladoire S, Laguerre B, Perrot V, Billard A, Escudier B, Gross-Goupil M. Real-world evidence of cabozantinib in patients with metastatic renal cell carcinoma: Results from the CABOREAL Early Access Program. Eur J Cancer. 2021 Jan;142:102-111. doi: 10.1016/j.ejca.2020.09.030. Epub 2020 Nov 27. PMID: 33253997.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#细胞癌#
40
#真实世界#
36
#转移性#
33
#转移性肾细胞癌#
41
#cabozantinib#
41
#ABO#
30
学习了
57