Libtayo提高了宫颈癌患者的生存率!
2021-03-15 Allan MedSci原创
赛诺菲和Regeneron的PD-1抑制剂Libtayo在晚期宫颈癌的III期临床试验中显示出阳性的总体生存(OS)结果。
赛诺菲和Regeneron的PD-1抑制剂Libtayo在晚期宫颈癌的III期临床试验中显示出阳性的总体生存(OS)结果。根据独立数据监测委员会(IDMC)的建议,将较早停止Libtayo(cemiplimab)治疗先前曾接受过化疗的复发/转移性宫颈癌患者的III期临床试验。
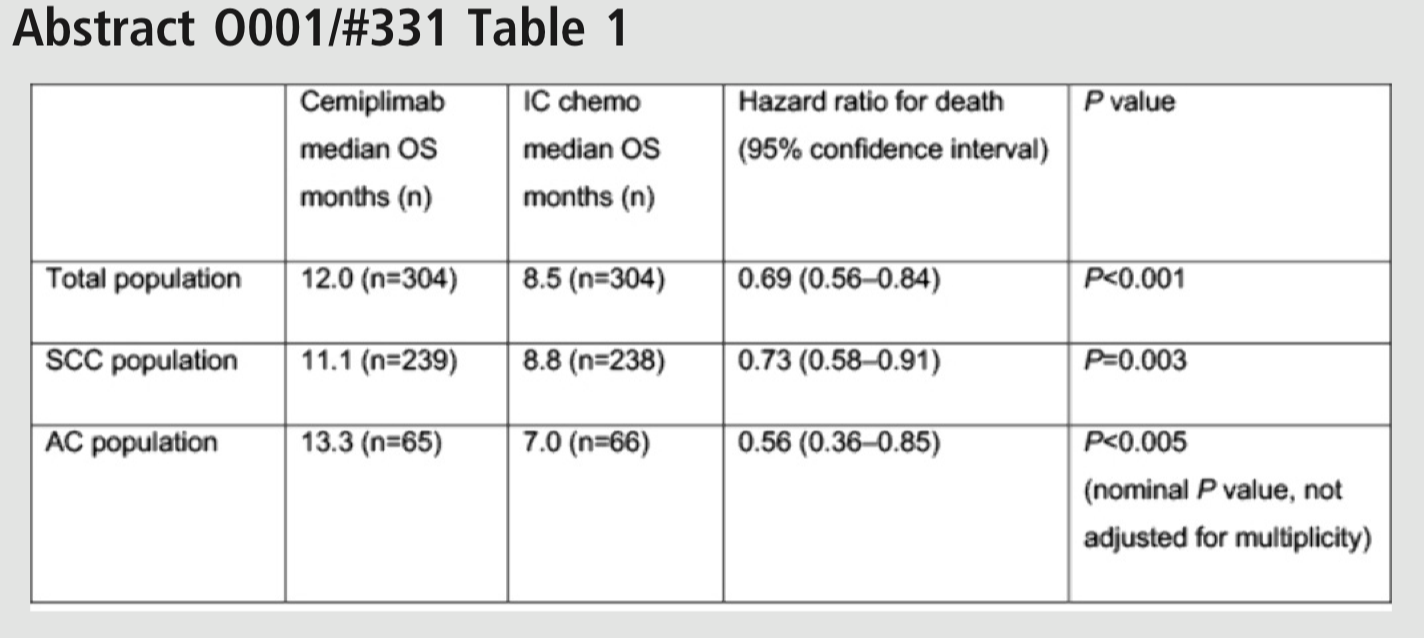
该试验招募了晚期宫颈癌患者。在总体人群中,接受Libtayo的患者的中位生存期为12.0个月,而化疗组患者的中位生存期为8.5个月,因此,Libtayo将死亡风险降低了31%。对于鳞状细胞癌患者,Libtayo将死亡风险降低了27%;而对于腺癌患者,Libtayo将死亡风险降低了44%。
IDMC建议在方案指定的中期分析后停止该试验,该试验发现Libtayo在提高宫颈癌患者OS方面非常显著。赛诺菲(Sanofi)和再生元(Regeneron)在一份声明中表示,这些数据将成为2021年向监管机构呈报的基础。此外,该试验的详细结果也将在即将举行的医学会议上发表。
Regeneron肿瘤转化和临床科学高级副总裁Israel Lowy表示:“众所周知,复发或转移性宫颈癌一线化疗后很难治疗,也没有批准的标准护理。这项试验显示,不论患者PD-L1状态如何,Libtayo都能帮助复发或转移性宫颈癌患者生存更长时间”。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#生存率#
40
#宫颈#
36
#Libtayo#
38
牛
91
很棒,学习了。
95
学习
82
学习了
89