Am J Otolaryngol:迷路内神经鞘瘤的前庭功能障碍和听力损失的治疗
2021-03-16 AlexYang MedSci原创
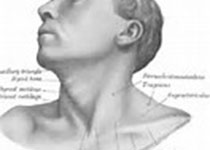
迷路内神经鞘瘤(ILS)是一种罕见的、良性的、缓慢生长的肿瘤,产生于骨迷路内的耳蜗或前庭神经的许旺细胞。
迷路内神经鞘瘤(ILS)是一种罕见的、良性的、缓慢生长的肿瘤,产生于骨迷路内的耳蜗或前庭神经的许旺细胞。 最近,有研究人员通过一个大型病例系列对该罕见的肿瘤治疗提供见解。 经机构审查委员会批准后,研究人员对2007年至2019年在研究人员所在单位治疗的所有ILS患者进行了回顾性病历审查。研究共有20名ILS患者(男9名,女11名)。9名患者的右耳受到影响(45%),11名患者的左耳受到影响(55%)。20名患者均认可主观听力损失。纯音平均值为72dB nHL。9例肿瘤(45%)为前庭内肿瘤,6例(30%)为耳蜗内肿瘤,4例(20%)为经经蜗轴肿瘤,1例(5%)为前庭蜗神经内肿瘤。3名患者(15%)使用助听器,2名(10%)使用BiCROS,2名(10%)使用CI,1名(5%)使用骨导植入。5名患者进行了前庭康复治疗。1名患者(5%)因顽固性眩晕通过经迷路入路进行了手术切除。没有患者接受放疗或脑内注射庆大霉素。 最后,研究人员指出,鉴于症状与其他疾病的相似性和有限的治疗方案,ILS在诊断和治疗上提出了挑战。听力损失可根据患者症状具体处理,而前庭损失可通过前庭治疗减轻。对于顽固性眩晕、严重
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#前庭功能障碍#
39
#听力#
22
#神经鞘瘤#
49
#功能障碍#
23
#前庭功能#
46