Cell Death Dis:KLF4-CD9/CD81-JNK信号通路失调促进肝癌发生发展
2020-05-21 QQY MedSci原创
外泌体是细胞外囊泡(EVs)的主要成分,是一种直径在30-150nm之间的纳米级膜结构,大多数的细胞类型都可以分泌这种结构。目前许多研究发现,外泌体可以通过转移不同的货物(包括蛋白质、DNA、micr
在癌症研究中,外泌体已被证实有助于肿瘤细胞的增殖、转移和信号转导过程。迄今为止,在大多数癌症类型中,对于外泌体表面分子的表达和重要性的研究还知之甚少,且其调控癌症发生发展的相关分子机制尚未完全了解。
既往研究发现,四次跨膜蛋白CD9和CD81通常被作为外泌体的表面标志物,参与肿瘤发生发展过程中细胞间的联系。KLF4则是各种癌症中的一个众所周知的肿瘤抑制因子。
该研究旨在揭示KLF4与CD9/CD81之间在肝细胞癌(HCC)中的关系。
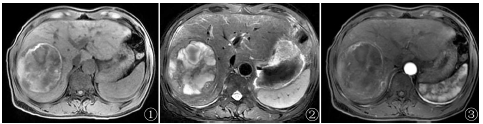
研究人员发现CD9和CD81能够被HCC细胞系中的KLF4转录激活。在大多数HCC肿瘤组织中,CD9和CD81的表达水平下降,且与癌症的晚期预后相关。此外,在肝癌标本中KLF4的表达水平与CD9和CD81的表达水平呈正相关。
功能研究发现,内外源过表达CD9和CD81均会抑制HCC细胞的增殖,而沉默CD9和CD81则表现出相反的结果。机制研究发现,JNK信号通路可能参与CD9和CD81介导的生长抑制作用。此外,KLF4、CD9或CD81的表达水平升高对HCC细胞外泌体的分泌没有显著的影响。
总而言之,该研究明确CD9和CD81是KLF4的新转录靶标,而KLF4-CD9/CD81- JNK信号转导通路的失调会促进肝细胞癌的发生发展,为治疗肝癌提供了新的潜在的靶标。
原始出处:
Li et al. KLF4-mediated upregulation of CD9 and CD81 suppresses hepatocellular carcinoma development via JNK signaling. Cell Death and Disease (2020) 11:299
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#发生发展#
35
#CEL#
31
#Dis#
29
#Cell#
30
#Death#
23
#信号通路#
27
#KLF4#
45
#CD8#
28
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
48