Radiology:基于磁共振弥散加权成像的虚拟弹性成像对肝纤维化的评估
2021-05-06 shaosai MedSci原创
众所周知,慢性肝病可发展为严重的肝纤维化和肝硬化。纤维化分级与如门脉高压、静脉曲张出血、肝性脑病和肝衰竭等多种并发症的发生相关。

众所周知,慢性肝病可发展为严重的肝纤维化和肝硬化。纤维化分级与如门脉高压、静脉曲张出血、肝性脑病和肝衰竭等多种并发症的发生相关。同时,肝硬化也是肝细胞癌的重要危险因素。多种研究表明,通过及早的干预及治疗可延缓甚至逆转肝纤维化的进展,因此对肝纤维化的早期发现并正确分期对改善预后至关重要。
肝活检是诊断肝脏疾病的金标准,然而该操作由于样本量小、病灶分布不均匀等原因可造成取样误差。MR弹性成像通过使用机械波测量组织弹性,在肝纤维化的分期方面的敏感性和特异性高达90%–99%。然而,由于需要复杂的机械设置、专用的MRI序列和长时间的图像采集,MR弹性成像在许多机构并不适用。
最近,临床上引入了一种基于DWI的通过将位移表观扩散系数(ADC)转化为组织弹性来进行无创肝分期的成像手段,已有研究表明,标准MR弹性成像得出的剪切模量和位移ADC产生的剪切模量可以等效地进行纤维化分期,因此可以直接从DW MRI估算肝组织剪切模量。
近日,发表在Radiology杂志的一项研究探讨了DW MRI和MR弹性成像对肝纤维化的分级及评价的诊断性能,为临床早期、准确地进行肝纤维化的评估提供了有价值的参考依据。
本项回顾性研究于2017年11月至2018年4月期间对所有纳入的患者进行了MR弹性成像和DW MRI扫描。由两个独立的阅读者从肝脏硬度图上的感兴趣区域获得每个患者的剪切模量(μMRE)。根据DW MRI (b = 200和1500 sec/mm2)计算位移表观扩散系数(ADC),并将其转换为基于DW MRI的虚剪切模量(μDiff)。根据μMRE和μDiff值(F0-F4)评估MRI肝纤维化分期,并评估血清纤维化标志物。统计分析包括Bland-Altman图、Bayesian预测和受试者工作特征分析。
本研究共纳入74例患者(平均年龄68岁±9岁[标准差];45名男性)。DW MRI的读者间可重复性系数为0.86 kPa, MR弹性成像的为1.2 kPa。位移ADC与μMRE之间具有很强的相关性(r2= 0.81;P < 0.001),μMRE和μDiff值(之间表现出极高的一致性(平均差值,-0.02 kPa±0.88;P <.001)。在55%的患者(41/74)中,以DW MRI为基础的纤维化分期与MR弹性成像为基础的分期相一致,35%的患者(26/74)在一个分期内存在差异。不显著(F0-F1)和显著纤维化(F2-F4)的二值化在85%的患者中显示出一致性(63/74;κ= 0.85)。与血清标志物(受试者工作特征曲线下面积[AUC],0.50 ~ 0.69)相比,μDiff在F0 ~ F2和F3 ~ F4期的鉴别上表现更好(AUC, 0.79;95%CI:0.69,0.90),而血清标记物在F0-F1和F2-F4的鉴别上表现稍好(使用MR弹性成像估计纤维化分期)。联合DW MRI与血清标志物显示出最高的鉴别性能(AUC,μDiff +天冬氨酸氨基转移酶/血小板比值:F0-F1 vs F2-F4, 0.81[95%CI:0.69,0.93],P = .17;F0-F2 vs F3-F4, 0.83[95%CI:0.74,0.92],P = .07;AUC μDiff + Fibrosis 4评分:F0-F1 vs F2-F4, 0.78[95%CI:0.64,0.92],P < .30;F0-F2 vs F3-F4, 0.81[95%CI:0.71,0.91],P = .08)。

图1 弹性图和纤维化图的生成示意图。磁共振弹性成像(MRE)得到的弹性图的示例(左上)。通过MRE计算软件,认为阴影部分是不可靠的。棕色区域对应用于分析的感兴趣区域(ROI)的位置。磁共振弥散加权成像(dMRI)获得同一层面的弹性和纤维化分期图(左下)。柱状图(中间)显示了上述感兴趣区域内(这里大多数体素属于F2类别)基于体素的纤维化阶段分布(dMRI)。所有获得的dMRI纤维化分期图(右)显示的各层面的同质性或异质性。
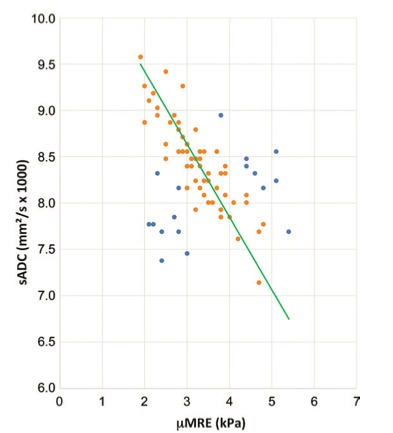
图2 扩散加权(DW) MRI位移表观扩散系数(sADC)与MR弹性成像(MR弹性成像)弹性的关系。位移ADC与MR弹性图剪切模量mMRE(单位:kPa)呈线性关系。绿色线对应于、报告的校准线(橙色数据点,±1标准差;蓝色数据点,>标准偏差)。
本研究结果表明,通过使用高b值位移表观扩散系数的扩散加权(DW)MRI得到的肝脏组织弹性与MR弹性成像的结果非常一致,表明该技术可用于肝纤维化的分期。因此,基于DW MRI的虚拟弹性成像是有创肝穿刺活检和常规MR弹性成像的有效替代手段。本研究同时为进一步有关该技术的标准化参数以及可重复性的相关研究铺平了道路。
原文出处:
Marie-Luise Kromrey,Denis Le Bihan,Shintaro Ichikawa,et al.Diffusion-weighted MRI-based Virtual Elastography for the Assessment of Liver Fibrosis.DOI:10.1148/radiol.2020191498
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#弥散加权成像#
37
#弹性成像#
30
#肝纤维#
33
已读,这真是受益匪浅呀!
60
#磁共振#
29
学习了
65