Heart:孤独与心血管事件之间的纵向联系
2020-06-20 MedSci原创 MedSci原创
该研究为孤独与心血管事件之间的关系提供了有力的证据。在心血管疾病的研究和干预措施中,孤独感应被视为CVD的社会心理危险因素。
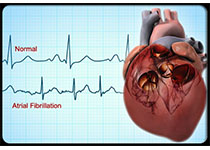
近日,心脏病领域权威杂志Heart上发表了一篇研究文章,这项研究旨在评估孤独症、社会隔离和心血管疾病(CVD)之间的关系,同时探究自我报告的CVD诊断和与CVD相关的住院人数。
该研究的数据来源于英国老年人纵向研究,并与行政医院记录和死亡登记数据相关联。用于分析自我报告CVD的分析样本量为5850人,从医院记录中提取的CVD样本为4587人,随访时间长达9.6年。研究人员使用生存分析对数据进行分析,以解决竞争风险事件。
受试者平均年龄为64岁(SD为8.3)。大约44%–45%是男性。在随访过程中,有17%的参与者报告有新诊断的CVD,16%的参与者为CVD相关住院。研究人员发现孤独与CVD事件的风险增加相关,而与潜在的混杂因素和风险因素无关。孤独感最强的人群CVD诊断的风险高出30%(HR:1.05,95%CI:1.01-1.09),而与CVD相关的住院治疗风险则高出48%(HR:1.08,95%CI :1.03-1.14),相比于孤独感最小的人群。几乎没有证据表明社会隔离与CVD诊断或入院风险独立相关。
由此可见,该研究为孤独与心血管事件之间的关系提供了有力的证据。在心血管疾病的研究和干预措施中,孤独感应被视为CVD的社会心理危险因素。
原始出处:
Feifei Bu.et al.Longitudinal associations between loneliness, social isolation and cardiovascular events.heart.2020.https://creativecommons.org/licenses/by/4.0/
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











牛逼
94
这个杂志投稿周期多久?
87
#血管事件#
23
#ART#
24
#HEART#
23