肝脏局灶性含脂病变的鉴别诊断集合
2018-08-26 佚名 熊猫放射
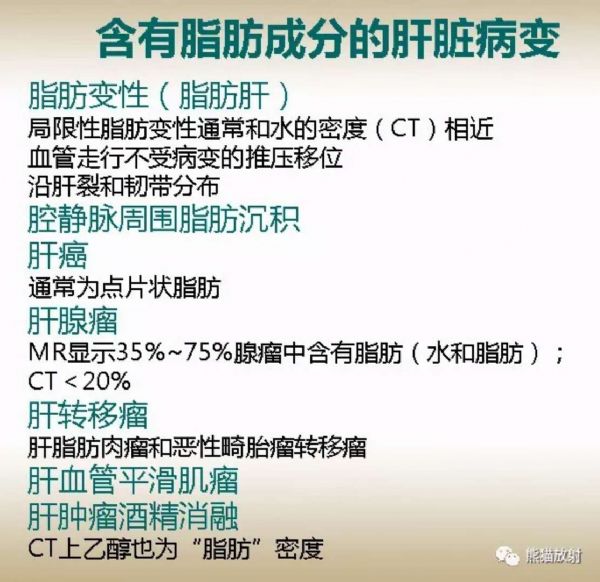
肝脏病变不管是良性病变还是恶性肿瘤,都可以含有脂肪,MRI对成熟脂肪甚至脂肪成分的检出具有独到的优势。
所含脂肪的表现形式
两种脂肪形式:
(1)病灶内含有不同量的成熟脂肪组织,主要由脂肪细胞构成,这类的病变主要有肝AML、肝脏脂肪瘤、肝癌术后网膜脂肪充填及肝包膜下假结节样脂肪浸润等,表现为化学位移成像反相位信号降低不明显,但脂肪抑制序列信号明显降低。
(2)病变组织发生脂肪变性,脂滴可出现于细胞内或细胞外间隙。这类病变本文中主要见于肝细胞腺瘤、局灶性脂肪肝、HCC等,表现为化学位移成像反相位信号降低,脂肪抑制序列不明显。
病灶内含有体积较大的成熟脂肪组织成分,则检出相对容易,而当病灶内仅含有体积很小的成熟脂肪组织或病灶内仅存在脂肪变性时,脂质成分的检出对MRI技术的应用就有更高的要求。
目前MRI的脂肪抑制技术有反转恢复序列、频率选择饱和法及同反相位序列3 种方法,各有优缺点。在临床实践过程中需要灵活运用MRI 脂肪抑制技术,从而提高脂肪检出率。
脂肪成分信号差异的病理学对照
早期HCC的脂肪变性多均匀分布于病变,表现为化学位移成像反相位信号降低,脂肪抑制序列不明显,呈细胞内脂肪微粒改变;而晚期可在HCC中形成脂肪瘤样改变,此时化学位移成像反相位信号降低不明显,但脂肪抑制序列信号明显降低,此时为相对较大的脂肪组织。
研究认为肝结节内脂肪成分的检出是腺瘤样退变结节转变为HCC的重要指征。HCC脂肪分布比较散在,呈镶嵌状,这与其病理基础相符合,为肿瘤中央发生坏死伴脂肪变性,故在病灶坏死区域内发生并呈散在分布。
文献报道肝腺瘤25%~40%有出血,30%~66%有假包膜,35%~90%的肝腺瘤T1WI 呈高信号,该高信号的病理基础为出血和含有不同程度的脂肪。
脂肪瘤、肝癌术后网膜脂肪填充及包膜下假结节样脂肪浸润均为相对较大脂肪组织,表现为CT即为负值密度,CT值-10Hu以下,MRI表现为典型的T1WI及T2WI高信号,化学位移反相位信号变化不明显,脂肪抑制序列为低信号。
肝脏含脂病变的MRI鉴别诊断
含脂HCC:
是原发性HCC的一种比较少见的特殊类型,由癌细胞脂肪代谢紊乱导致。有一些特征性影像学表现:
(1)含脂肝细胞肝癌多位于肝脏边缘;
(2)脂肪变性细胞主要以斑片状形式散在分布于病灶周围区域,中心区域相对少见;
(3)“快进快出型”强化,动脉期可见扭曲强化血管影及不规则的强化分隔,延迟期分隔强化减退程度不明显,病灶边缘包膜逐渐强化。
当HCC较小时,可因脂肪变性而使病变密度降低,是由于早期HCC的脂肪变性多呈均匀分布所致;患者多有慢性肝病史、AFP阳性、假包膜显示,局部病变可见胆管扩张改变。
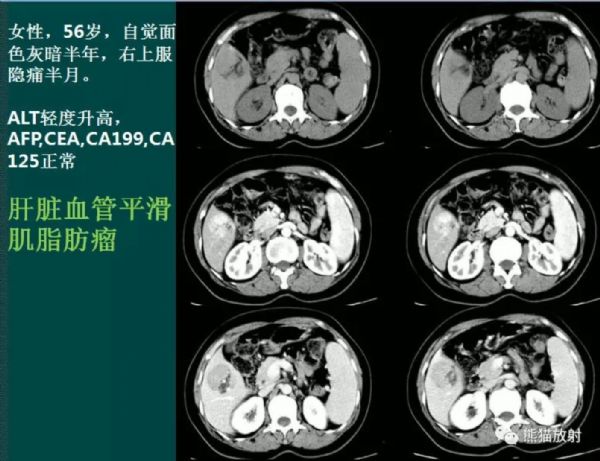
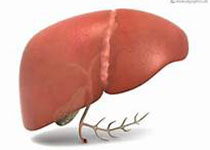
AML:
AML内脂肪含量5%~90%不等,其中乏脂型HAML内脂肪含量<10%。脂肪成分以团块状表现为主,管状大血管以大静脉湖为主,所以动态增强强化血管影多在门静脉期达到强化峰值,病灶以延迟强化为主而脂肪组织无强化。病灶内的非脂肪成分常表现为明显的早期和延迟强化,呈“快进慢出”的增强模式。
肝腺瘤:
约占肝脏良性肿瘤的1.6%,是一种少见的、易出血的,并具有潜在恶性倾向的肿瘤。脂肪变性区域CT的显示率不到10%,有文献报道用MRI梯度双回波序列显示肝腺瘤肿瘤脂肪变性发生率高达90%。
肿瘤好发于年轻女性,与正常肝组织分界清晰,周围常见低密度“透明环”,瘤内易伴发出血或坏死以及脂肪变性使MRI信号复杂多变、混杂;动态增强动脉期可见肿瘤供血动脉与明显强化的病灶相连,肿瘤实性部分显著较均匀强化。
肝硬化结节脂肪沉积:
在肝退变结节(DN) 和小肝癌( HCCs)中均可出现脂肪沉积;其与原发性含脂肝细胞肝癌主要区别是肝硬化背景下的小结节(直径<3cm),对肝硬化结节脂肪沉积的随访动态观察是区别原发含脂HCC的有效手段之一。
透明细胞性肝癌:
发病率不足HCC的10%,是HCC的一种少见的临床病理类型。由于癌细胞胞质内因富含糖原而呈透明状,当癌细胞中透明细胞比例超过50%时,应诊断为透明细胞。其影像学表现形式无明显特异性,依靠影像学检查难以与含脂HCC鉴别,其确诊和鉴别需依赖病理和免疫组织化学检查。
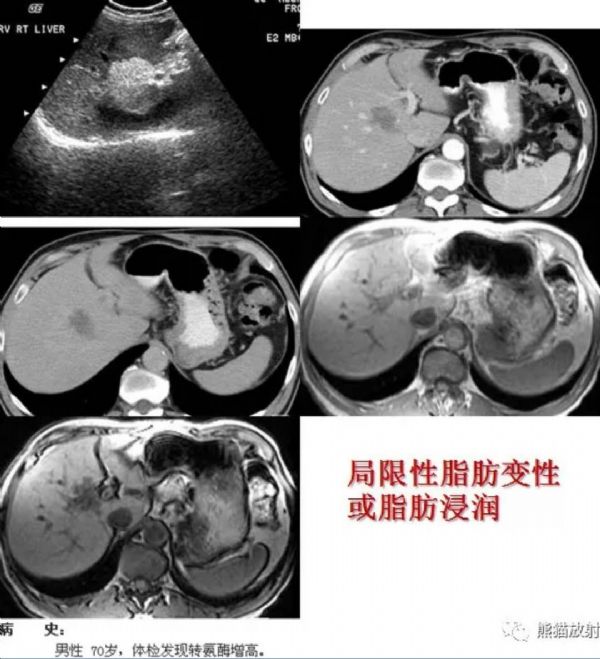
假结节样脂肪浸润:
多见于局灶性脂肪肝或弥漫性脂肪肝背景下,表现为肝内低密度结节影,无占位效应,增强扫描均匀强化,病灶内有正常血管穿行,其强化形式与正常肝脏组织一致。
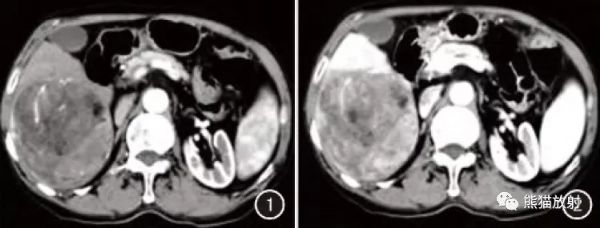
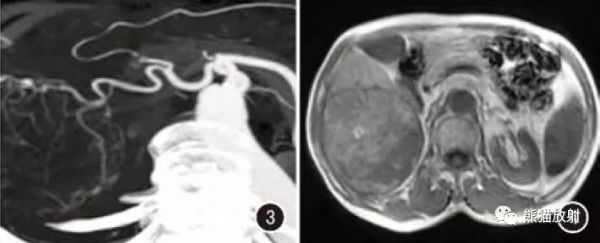
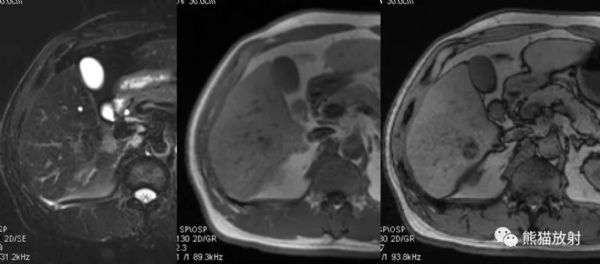
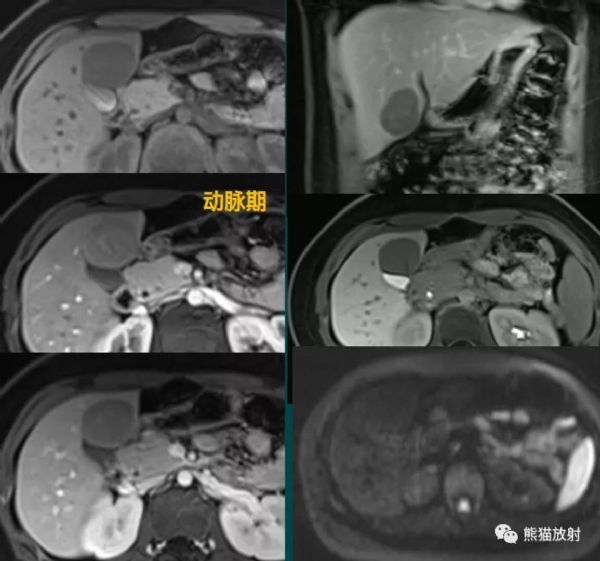
↑ 含脂肝细胞肝癌。脂肪以斑片状主要出现于病灶周围区域,动态增强动脉期( 图1) 病灶明显强化,并见强化扭曲血管影,门静脉期强化减退( 图2) ,CTA( 图3) 示肿瘤由肝固有动脉新生分支血管供血为主。脂肪信号在同反相位( 图4、5) 上显示更加清晰和敏感,并且含脂区域以位于肿瘤外周区域为主;脂肪区域在DWI 像上显示敏感,呈明显低信号(图6)。
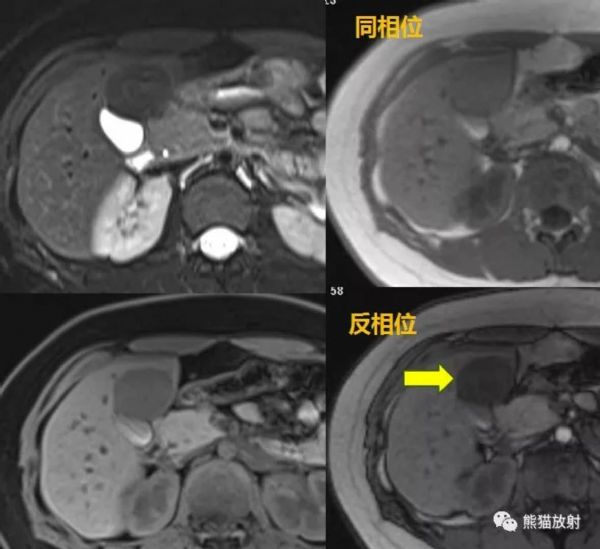
↑ 男 50岁,肝细胞肝癌。B超发现肝占位,乙肝十余年,AFP不高。CT平扫密度低,T2WI-FS呈等信号,MR反相位信号减低,增强扫描“快进快出”。
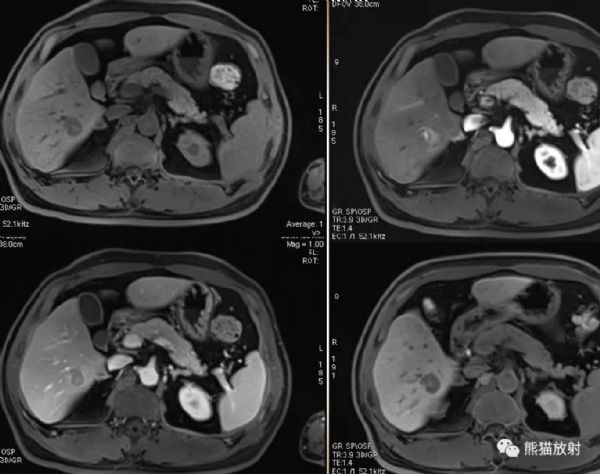
↑患者女性,16岁;肝细胞腺瘤伴弥漫重度脂肪变性。病灶呈长T1短T2信号,反相位示病灶信号减低;DWI无明显弥散受限;增强扫描动脉期轻度强化,门脉期及延迟期强化程度减低,肝胆特异期呈明显低信号。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#局灶性#
42
学习了
86
#鉴别诊断#
33
读书百遍其义自见,多看多读总有好处
68
认真学习,不断进步,把经验分享给同好。点赞了!
63
学习了
76