JAHA:急性心肌梗塞患者发生早期复发性心肌梗塞的特征和结局
2021-08-02 MedSci原创 MedSci原创
早期RMI是一种危及生命的疾病,5年内死亡率接近50%。支架相关事件和冠状动脉疾病进展是大多数早期RMI的原因。药物依从性、积极的危险因素管理和治疗过渡应该是预防早期RMI的基石。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员旨在了解急性心肌梗死后出院90天内因复发性心肌梗死(RMI)再次入院患者的特征和结局。
研究人员分析了2010年1月1日至2017年1月1日期间急性心肌梗死后90天内因早期RMI入院的所有患者再梗死的时间、病因和结局。研究人员共确定了6626例急性心肌梗死住院患者,其中在出院90天内发生了168例RMI。
患者的平均年龄为65.1±13.1岁,37%为女性。早期RMI的90天再入院率为2.5%。黑人、医疗管理、较高的肌钙蛋白T水平和较短的住院时间是早期RMI的独立预测因素。
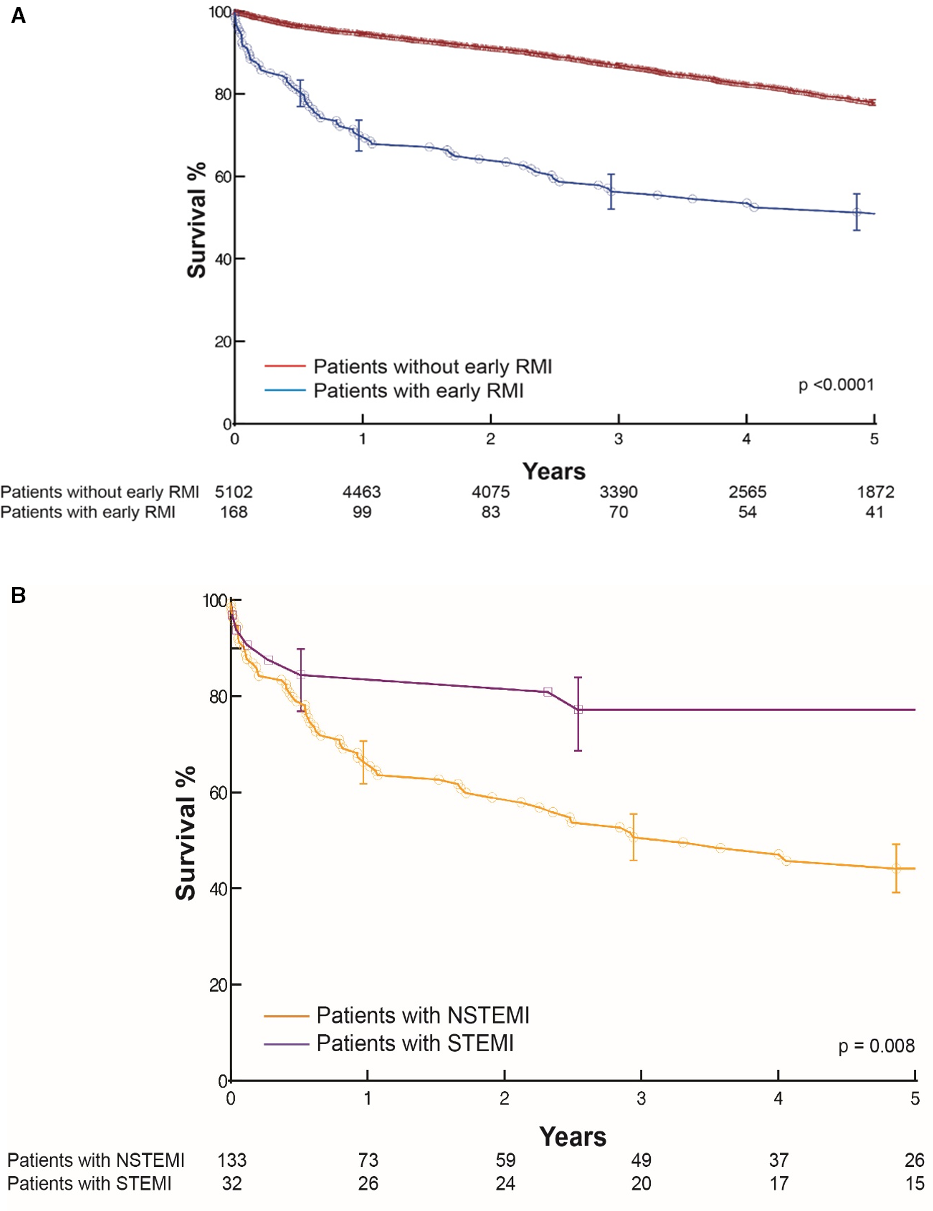 早期复发性心肌梗塞患者的结局
早期复发性心肌梗塞患者的结局
与经皮冠状动脉介入治疗(P=0.04)或冠状动脉旁路移植术(P=0.2)相比,药物治疗组发生早期RMI的风险更高。再梗死的主要机制是支架内血栓形成(17%)、疾病进展(12%)和病情未发生改变的冠状动脉疾病(11%)。5年时,早期RMI患者的全因死亡率为49%(95%CI为40%-57%),而无早期RMI患者的全因死亡率为22%(95%CI为21%-23%)(P<0.0001)。
由此可见,早期RMI是一种危及生命的疾病,5年内死亡率接近50%。支架相关事件和冠状动脉疾病进展是大多数早期RMI的原因。药物依从性、积极的危险因素管理和治疗过渡应该是预防早期RMI的基石。
原始出处:
Raunak Nair.et al.Characteristics and Outcomes of Early Recurrent Myocardial Infarction After Acute Myocardial Infarction.JAHA.2021.https://www.ahajournals.org/doi/full/10.1161/JAHA.120.019270
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#早期复发#
39
#复发性#
35
#AHA#
40
#急性心肌梗塞#
49
学习
71