Neurology: 脑淀粉样血管病变相关炎症的进展和预后如何?
2021-09-18 MedSci原创 MedSci原创
这些来自最大的CAA-ri患者纵向队列登记的结果,支持该疾病的临床-放射学急性表现的短暂和潜在复发的炎症性质
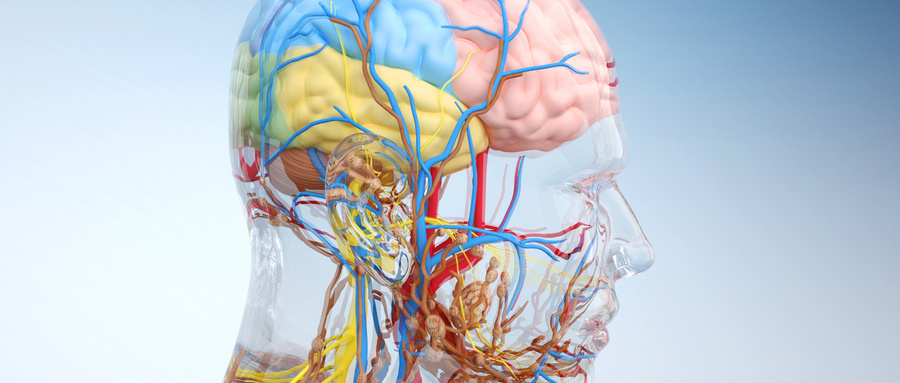
大脑淀粉样血管病变相关炎症(Cerebral amyloid angiopathy-related inflammation,CAA-ri)是一种罕见的自身免疫性脑病,与脑脊液中针对沉积在皮质和脑膜动脉、小动脉和毛细血管壁上的淀粉样β(Aβ)蛋白的自身抗体浓度增加有关。
该病的特点是急性/亚急性的神经系统症状,从非常轻微的认知障碍和头痛到快速进行的认知能力下降、癫痫发作、精神状态改变和局灶性神经功能障碍。
这些神经系统症状与磁共振成像(MRI)上提示血管性水肿(VE)的急性白质高信号(WMHs)有关,与CAA的MRI特征如脑微出血(CMBs)和皮质浅层蜘蛛网病(cSS)有关。
明确的CAA-ri的诊断需要组织病理学的确认。然而,最近的临床放射学标准和脑脊液(CSF)中检测抗Aβ自身抗体的超灵敏测试,大大增加了目前的诊断能力,减少了对有创脑活检的需要。
有证据表明,CAA-ri是一种潜在的可逆性疾病,对免疫抑制疗法有反应,但这仅限于稀少的病例报告或来自单个中心的小型回顾性病例系列。
虽然CAA-ri被认为只限于CAA患者,但该病现在越来越多地被认识和诊断为不同的神经系统和神经放射学表现,包括在阿尔茨海默病(AD)的免疫临床试验中观察到的与淀粉样蛋白相关的影像学异常(ARIA)的惊人的相似性。
使用抗Aβ单克隆抗体的治疗因以下情况而变得复杂:
1)ARIA-E(水肿),包括提示实质水肿和/或渗出的WMH局域,
2)ARIA-H(出血),包括CMBs和cSS。
鉴于临床试验的样本和数据非常少,CAA-ri中自发发生的ARIA(ARIA样)被提议作为研究此类试验中治疗诱发的ARIA的有效模型。这使人们建立了一个合作研究框架,即 "炎症性脑淀粉样血管病和阿尔茨海默病βiomarkers(iCAβ)国际网络 "倡议(Inflammatory Cerebral Amyloid Angiopathy and Alzheimer’s disease βiomarkers (iCAβ) International Network),旨在:
1)提高诊断、预后和治疗能力
2)减少这些未被充分认识的疾病管理中的变异性。
藉此,意大利米兰大学的Laura Antolini等人,探究了CAA-ri的自然史,并为与皮质激素治疗相关的结果提供新的证据,该研究是通过iCAβ国际网络倡议系统地招募,首次诊断为CAA-ri的定义明确的患者来开展。
在2013年1月至2017年3月期间,他们通过iCAβ国际网络招募了符合CAA-ri诊断标准的住院患者,这是一项多中心、基于医院的纵向、前瞻性观察研究。在3、6、12、24个月的随访中,采用了在首次就诊和随后的亲自访问中系统收集数据的方案,包括在1.5T MRI上获得的T1加权、GRE-T2*、流体抑制T2加权(FLAIR)和T1后钆对比增强图像。核磁共振图像的集中阅读是在对临床、治疗和时间点信息保密的情况下进行的。主要结果是生存率、临床和放射学恢复、脑内出血(ICH)和CAA-ri的复发。
结果
本研究共纳入113名参与者(10.6%明确,71.7%可能,17.7%可能为CAA-ri),平均年龄72.9岁,43.4%为女性,37.1%为APOEε4携带者。36.3%有阿尔茨海默病史,33.6%有ICH病史。
ICH病史以及随访时新ICH的发生在基线时有皮质浅层蛛网膜病变的患者中更为常见(分别为52.6% vs 14.3%; p< 0.0001和19.3% vs 3.6%; p<0.009)。
首次出现CAA-ri后,70.3%(95%CI,61.6-78.5)和84.1%(95%CI,76.2-90.6)在三个月和十二个月内临床康复,随后分别有45.1%(95%CI,36.4-54.8)和77.4%(95%CI,67.7-85.9)放射学康复。
在首次发作的临床放射学指标恢复后,38.3%(95% CI,22.9 - 59.2)在随后的24个月内至少有一次复发。如果突然停止静脉注射大剂量皮质类固醇脉冲治疗,与缓慢的口服减量相比,复发的可能性更大(危险比4.68;95% CI,1.57-13.93;p=0.006)。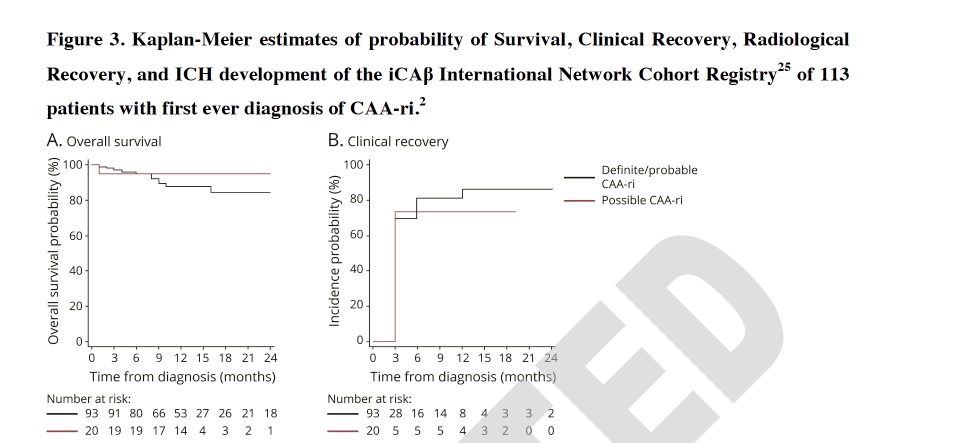
这些来自最大的CAA-ri患者纵向队列登记的结果,支持该疾病的临床-放射学急性表现的短暂和潜在复发的炎症性质,以及静脉注射皮质类固醇脉冲治疗后缓慢口服减量对预防复发的有效性。该结果强调了在Aβ驱动的疾病中对自发性ARIA样事件进行鉴别诊断的重要性,包括阿尔茨海默病患者暴露于免疫治疗药物的治疗相关ARIA。
原文出处:
Antolini L, DiFrancesco JC, Zedde M, et al. Spontaneous ARIA-like Events in Cerebral Amyloid Angiopathy–Related Inflammation: A Multicenter Prospective Longitudinal Cohort Study. Neurology. Published online September 16, 2021:10.1212/WNL.0000000000012778. doi:10.1212/WNL.0000000000012778
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#血管病#
44
#脑淀粉样#
45
#预后如何#
39
#Neurol#
44
#血管病变#
50
#脑淀粉样血管病#
50
已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读
43