Diabetologia:1型糖尿病心血管健康指标可能预示心血管事件的发生
2022-04-23 从医路漫漫 MedSci原创
患有1型糖尿病的男性患心血管并发症的风险是普通人群中男性的4倍,而患有1型糖尿病的女性患心血管并发症的风险是普通人群中女性的8倍。
背景:心血管疾病(CVD),如心肌梗塞和中风,是糖尿病最重要的并发症之一。尽管全球1型糖尿病人群的心血管并发症发生率有所下降,但这些糖尿病患者的并发症风险高于普通人群。患有1型糖尿病的男性患心血管并发症的风险是普通人群中男性的4倍,而患有1型糖尿病的女性患心血管并发症的风险是普通人群中女性的8倍。然而,有心血管并发症高风险的1型糖尿病患者可能受益于生活方式的改变,以降低他们患心血管疾病的风险。
美国心脏协会(AHA)公布了理想心血管健康的标准,确定了七项指标:吸烟、BMI、体力活动、饮食、总胆固醇、血压和空腹血糖。根据文献和以前委员会的建议,对这些心血管健康指标中的每一项的理想值进行了指定。根据理想心血管健康指标的数量进行评分,在普通人群中的研究表明,得分越高,心血管疾病的风险越低。以前的研究已经检查了1型糖尿病患者的理想心血管健康,但使用的标准和阈值并不总是与AHA使用的标准和阈值相同。事实上,对于1型糖尿病患者,使用糖化血红蛋白比空腹血糖和总胆固醇/高密度脂蛋白胆固醇比总胆固醇更适合作为心血管健康指标.
Alman等人关于理想健康指标的第一次研究使用了心血管疾病的替代标记物,并没有关注主要的心血管结果。一项横断面研究评估了这些指标的普及率,还发现动脉僵硬(脉搏波速度、臂部扩张性和增大指数)随着理想健康指标数量的增加而降低。一项横断面和前瞻性研究评估了冠状动脉钙化(CAC)的患病率和进展。作者发现,心血管健康指标的聚集性越大,CAC的患病率和进展就越低。McCarthy等人发表了两项关于1型糖尿病患者心血管健康指标的横断面研究,以探索这些指标的患病率及其与社会人口统计学变量的关系。Rawshani等人通过聚集危险因素检查了发生心血管事件的风险,比较了患有和不患有1型糖尿病的人。他们专注于五项指标-吸烟、血压、低密度脂蛋白-胆固醇、糖化血红蛋白和蛋白尿-并为瑞典人选择了风险阈值。他们发现,在平均10年的随访中,急性心肌梗死、糖尿病、心力衰竭和中风的发病率逐渐增加,指标没有达到目标水平的数量也有所增加。
目的:这项前瞻性研究的目的是检验(1)心血管健康指标良好的人群和(2)通过对这些指标进行分类来降低1型糖尿病患者的心血管疾病风险。
方法:对参加EURODIAB前瞻性并发症研究的2313名受试者的资料进行分析。所有患者均患有1型糖尿病(51%的男性,平均年龄为32±9岁)。研究人员对七项心血管健康指标--吸烟、BMI、体力活动、饮食评分、总胆固醇/高密度脂蛋白-胆固醇比率、收缩压和舒张压以及糖化血红蛋白进行了研究,将其分为有利和不利两类。使用COX比例风险模型计算每个指标的心血管事件发生率(95%CI)。根据有利指标的数量对每个个体进行评分,从而形成集群。
结果:在平均(7.2±1.3)年的随访期内,共有163人发生心血管事件。与HbA1c水平较差的参与者相比,HbA1c水平较好的参与者心血管风险显著降低37%(HR[95%CI]0.63[0.44,0.91]),而血压较好的参与者(收缩压<112 mm Hg,舒张压<70 mm Hg)的心血管风险显著降低44%(HR[95%CI]0.56[0.34,0.92])。在观察到较低的HR时,较有利的指标具有更大的聚集性,存在剂量-反应关系:与没有有利指标的人相比,具有四个或更多有利指标的人的HR为0.37(95%可信区间0.18,0.76),在糖尿病诊断时根据性别和年龄进行了调整。
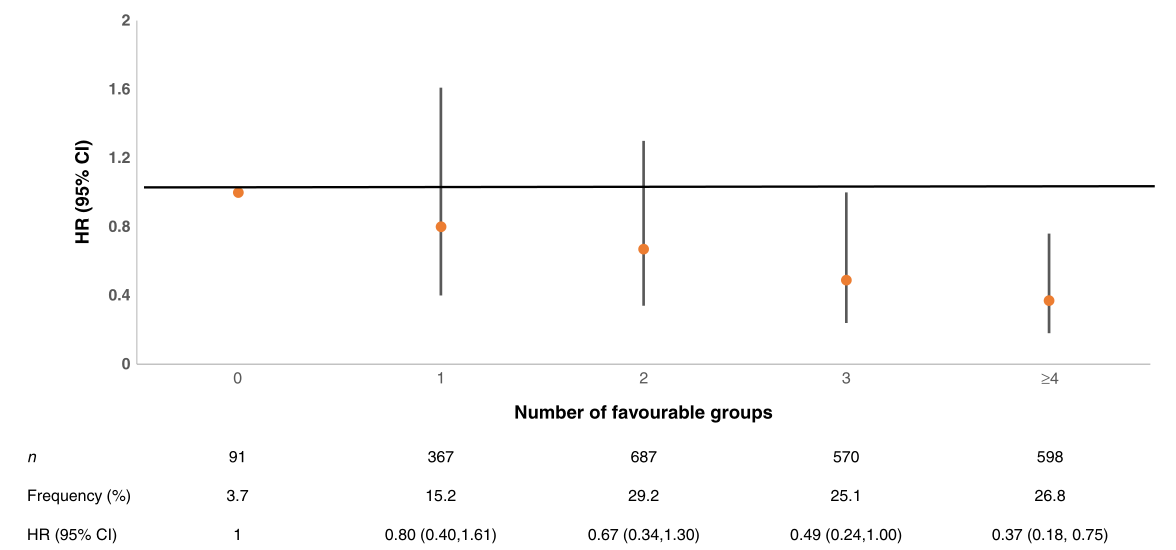
图1心血管事件的比率(95%CI),根据输入数据的模型中最有利的心血管健康指标组或三分位数的数量,根据糖尿病诊断的年龄和性别进行调整:EURODIAB前瞻性并发症研究
表1 EURODIAB对1型糖尿病患者的研究中参与者的基线特征,按心血管疾病状况分类
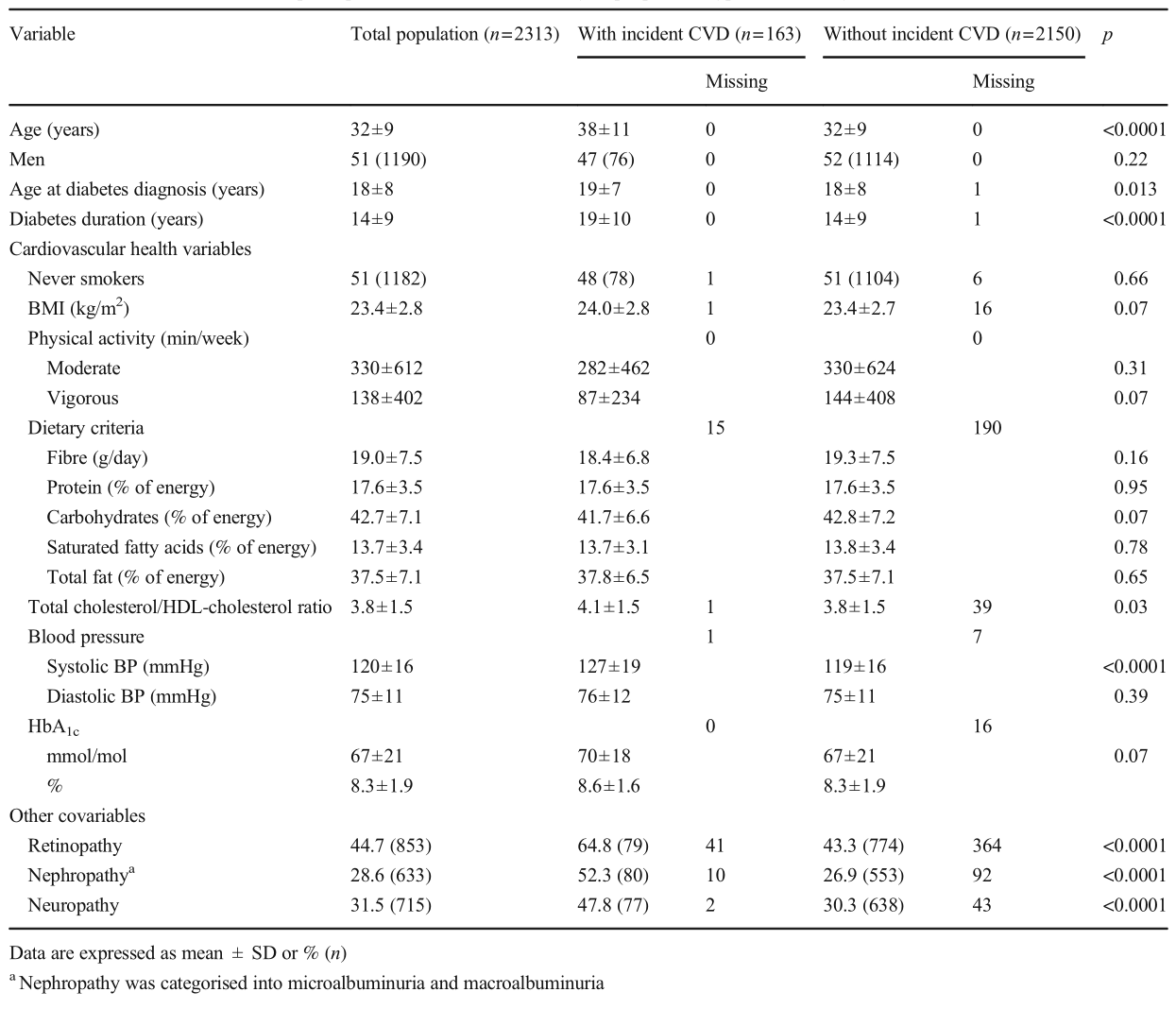
结论:在我们的研究中,低HbA1c和低血压是1型糖尿病患者心血管健康的保护性指标。以所有心血管健康指标为目标可能比以单一指标为目标更有效地预防心血管疾病。
原文出处:Soulimane S, Balkau B, Vogtschmidt YD,et al.Incident cardiovascular disease by clustering of favourable risk factors in type 1 diabetes: the EURODIAB Prospective Complications Study.Diabetologia 2022 Apr 12
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#糖尿病心血管#
35
#BET#
36
#血管事件#
42
#DIA#
31
#健康指标#
0
学到了
54