Clin Oral Investig:微创手术可有效治疗牙周炎导致的骨内缺损
2022-05-13 sunshine MedSci原创
牙周炎是由多种致病菌引起的炎症性疾病,会导致临床附着水平(CAL)和骨内缺损。有学者提出使用微创手术技术(MIST)来治疗孤立的骨内缺损。
牙周炎是由多种致病菌引起的炎症性疾病,会导致临床附着水平(CAL)和骨内缺损。有学者提出使用微创手术技术(MIST)来治疗孤立的骨内缺损,其主要原则是使用最小化皮瓣、保留乳头技术和改良的内侧褥式缝合来实现无张力的伤口闭合。已有研究报道,单独的微创手术以及联合再生材料都能很好的治疗牙周炎骨内缺损。然而,再生材料在微创手术中是否有额外的益处尚不清楚。近日,发表于Clin Oral Investig的一项随机对照试验中,研究人员改良了MISTms,并探究了其在治疗骨内缺损时使用和不使用再生材料的疗效,并确定了影响改善1年CAL的因素。

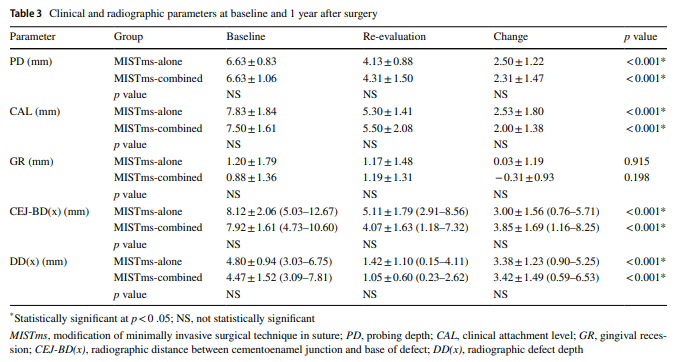
研究共纳入36名牙齿骨内缺损的患者,随机分配到MISTms(单独组,18名患者)或MISTms加去蛋白牛骨矿物质和胶原膜(联合组,18名患者)。在1、2、3和6周时,通过早期愈合指数(EHI)评估伤口愈合。基线和术后1年记录探诊深度(PD)、CAL、牙龈退缩、X线示缺损深度以及从缺损底部到牙釉质牙本质交界处的距离。基于CAL增加和手术后PD的组合,评估了一年的综合结果指标。对影响1年CAL增益的因素进行了分析。
结果显示,单独组的15名患者和联合组的16名患者完成了研究。单独组在1周内的伤口愈合情况明显较好。单独组和联合组的CAL明显增加,分别为2.53±1.80 mm和2.00±1.38 mm。影像学上的骨量增加分别为3.00 ± 1.56 mm和3.85 ± 1.69 mm。然而,两组之间关于1年的综合结果没有明显差异。较低的EHI(最佳伤口愈合)和较高的基线CAL对1年的CAL增益有积极影响。
综上所述,该研究结果表明,MISTms是治疗骨内缺损的一种有效方法。再生材料对术后1年综合结果没有显示出额外的有益之处,早期切口愈合和基线CAL是影响1年CAL增加的因素。
原始出处:
Bei Liu, et al., Efficacy of periodontal minimally invasive surgery with and without regenerative materials for treatment of intrabony defect: a randomized clinical trial. Clin Oral Investig. 2022 Feb;26(2):1613-1623. doi: 10.1007/s00784-021-04134-w.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Oral#
26
#EST#
40
#微创手术#
38
#微创#
41
#牙周#
52
#有效治疗#
49