OCC 2022:PIANO评分在急性心肌梗死预后评估和指导急诊PCI术血栓抽吸中的临床价值
2022-05-25 梅斯医学整理 梅斯医学整理
对于急性心肌梗死行急诊PCI术的患者,PIANO评分存在一定的预后价值。另外,PIANO评分可能有助于指导急诊PCI术中血栓抽吸。
在既往研究中,科学家们建立了一种急诊PCI术中无复流现象发生的预测评分系统-PIANO评分。来自复旦大学附属中山医院心内科团队,进一步探究了PIANO评分在急性心肌梗死预后评估和指导急诊PCI术血栓抽吸中的临床价值。
研究人员收纳了来自2009年至2018年于我院心内科行急诊PCI术的急性心肌梗死患者,并进行临床随访。终点事件定义为术后2年的全因死亡。通过Cox比例风险模式探究PIANO评分和临床预后的关系,并采用倾向评分校正混杂因素的作用。采用限制性立方样条图评估PIANO评分的大小和随访2年全因死亡率之间的关系。
结果显示:在入组2312例患者中,其中52.3%有高(≥8分)PIANO评分。术后随访2年,高PIANO评分患者更容易发生全因死亡,尤其是在第1个月。限制性立方样条图分析表明,PIANO评分的大小和随访2年全因死亡率之间存在线性关系。
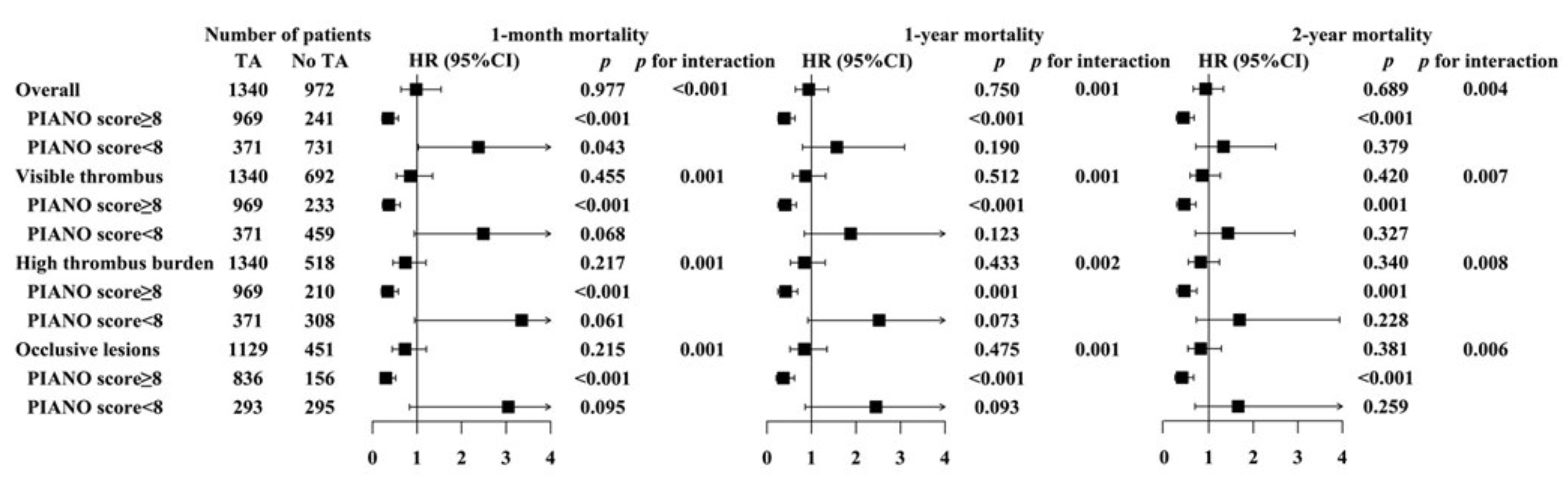
进一步分析表明,在总体人群或存在可见血栓、高血栓负荷、血管比塞的人群中,采用血栓抽吸均未改善临床预后。然而,在高PIANO评分的人群中采用血栓抽吸,可明显改善临床预后。
总之,对于急性心肌梗死行急诊PCI术的患者,PIANO评分存在一定的预后价值。另外,PIANO评分可能有助于指导急诊PCI术中血栓抽吸。
资料来源:2022 第16届东方心脏病学会议
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#PCI术#
51
#临床价值#
34
#血栓抽吸#
48
#急诊PCI#
36
#预后评估#
46
#OCC#
41