PNAS:胰岛素的折叠瓶颈或使大多数人易患2型糖尿病
2020-11-07 MedSci原创 MedSci原创
科学家发现,胰岛素已经遇到了进化的死胡同,限制了它适应肥胖的能力,从而使大多数人容易患2型糖尿病。
最近,一项来自印第安纳大学医学院、密歇根大学和凯斯西储大学的新研究已确定,胰岛素序列已经在生产能力受损的边缘根深蒂固,这种内在的脆弱性被导致儿童糖尿病的胰岛素基因的罕见突变所掩盖。这项研究利用生物物理学的概念和方法,将蛋白质化学与新兴的进化医学领域联系起来。

胰岛素是由一系列高度特异的过程产生的,这些过程发生在被称为β细胞的特殊细胞中。关键的一步是折叠一种叫做胰岛素原的生物合成前体,以实现激素的功能性三维结构。过去的研究表明,受损的生物合成可能是多种突变的结果,阻碍了原胰岛素的可折叠性。
这个小组试图确定在包括人类在内的脊椎动物体内胰岛素的进化是否遇到了障碍。是否有一系列复杂的步骤限制了胰岛素的序列,使其无法折叠?如果是这样的话,这是否会使人类更容易患上2型糖尿病,成为现代社会的一种流行病。根据发表在《美国国家科学院院刊》(Proceedings of the National Academy of Sciences)上的这项研究,答案是肯定的。
脊椎动物胰岛素- igf家族的进化为研究蛋白质在严格选择下的遗传变异提供了一个模型。目前的研究已经确定了不变芳香残基(PheB24)对新生的可折叠性的一个重要的贡献,并证明了这一贡献与残基直接参与激素受体界面一样重要。突变的人类胰岛素功能在动物胰岛素的自然变异范围内,但这种突变已经被进化排除在外。这个看似矛盾的答案是,被禁止的突变选择性地阻止了原胰岛素的折叠,并对细胞造成压力。
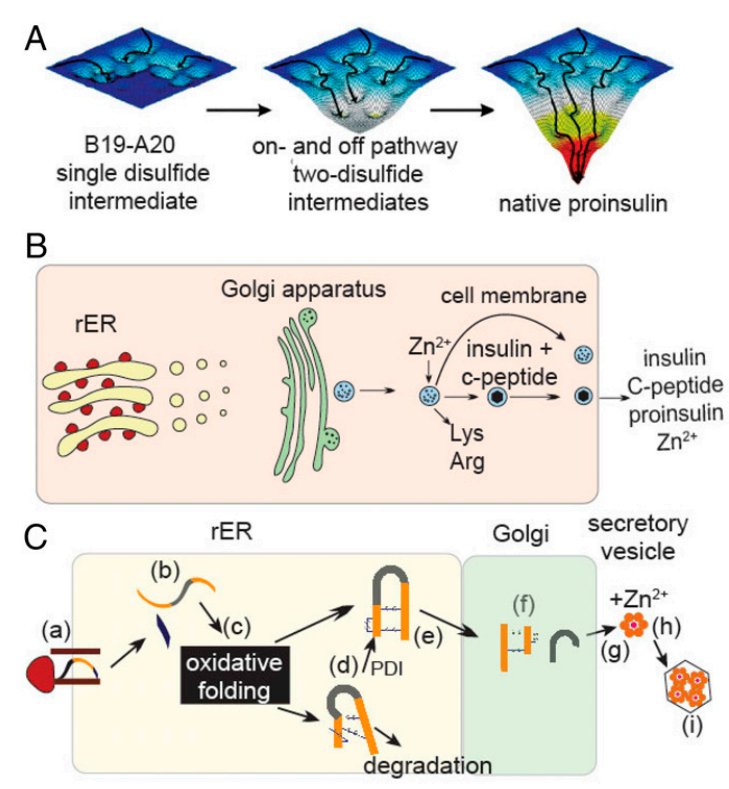
胰岛素原的折叠及其生物合成途径
研究小组发现,即使是最轻微的胰岛素测序过程的变化,也会损害胰岛素折叠(以及最终的胰岛素分泌),而且还会诱发细胞应激,导致β细胞功能障碍,最终导致永久性损伤。
这项研究强调了折叠效率的重要性,它是过去5.4亿年来胰岛素进化过程中一个关键但隐藏的因素。人类已经进化到容易受到胰岛素基因不同突变的影响,这种脆弱性是一种罕见的单基因型糖尿病的基础,并为目前与肥胖相关的糖尿病流行提供了进化背景。
专家们一致认为,这一发现为更好地了解成人和儿童2型糖尿病的发展提供了关键见解。在印第安纳州和世界各地,2型糖尿病都在以惊人的速度增长。
“这项研究是阐明影响胰岛素合成和功能的结构生物学关键因素的力作,”哈佛医学院乔治R.米诺特医学教授Barbara Kahn说。作者强调了一个事实,即胰岛素基因在整个进化过程中容易发生突变,从而损害胰岛素的功能或使细胞处于应激状态。当我们接近发现胰岛素100周年的时候,这些观察可能会引导我们更好地理解2型糖尿病的发病机制。
Philipson教授指出:“目前的发现确定了未来的一个主要问题:在携带INS基因变异的患者中所见的有害的胰岛素原异常折叠是否也会发生,也许是在较低的水平,但在世界各地的2型糖尿病患者中更广泛。”
接下来,该小组将致力于充分确定使胰岛素原在细胞中可折叠的序列决定因素。他们的希望这项工作将最终能促使一种新型药物的出现,这种药物可以减轻胰岛素原不稳定的可折叠性引起的细胞应激,并针对β细胞中的细胞应激,从而为高危患者保留胰岛功能。
参考文献:Nischay K. Rege, et al . Evolution of insulin at the edge of foldability and its medical implications. PNAS, 2020 DOI: 10.1073/pnas.2010908117
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PNAS#
36
#胰岛#
36
文章很实用
74
好好学习!
71
谢谢MedSci提供最新的资讯
43