Br J Cancer:调节性T细胞可预测软组织肉瘤患者的临床结果
2021-06-15 xiaozeng MedSci原创
肿瘤微环境(TME)由多种细胞类型(如免疫细胞、成纤维细胞)和细胞外成分(如激素、细胞因子、生长因子)组成,其在宿主对肿瘤的免疫反应过程中起着至关重要的作用。
肿瘤微环境(TME)由多种细胞类型(如免疫细胞、成纤维细胞)和细胞外成分(如激素、细胞因子、生长因子)组成,其在宿主对肿瘤的免疫反应过程中起着至关重要的作用。
抗肿瘤反应的程度取决于T细胞抑制和激活信号之间的平衡,该过程主要通过免疫检查点标志物所介导。而在TME内,包括PD-1(程序性细胞死亡蛋白1)及其配体PD-L1在内的特定免疫检查点标志物的异常表达,通常会促进免疫耐受和肿瘤细胞的免疫逃逸。
既往研究显示,T细胞表面PD-1的表达升高以及PD-L1/PD-1通路的连续过度激活可减轻调节性T细胞(Tregs)的凋亡,并增强抗原特异性T细胞的凋亡。
软组织肉瘤(STS)通常被认为是非免疫原性的,尽管其特定的亚型对免疫疗法有反应。该研究旨在分析STS中肿瘤浸润淋巴细胞(TIL)和免疫检查点标志物,并评估其对该疾病的局部复发(LR)、远端转移(DM)以及患者的总生存期 (OS) 的预后影响。
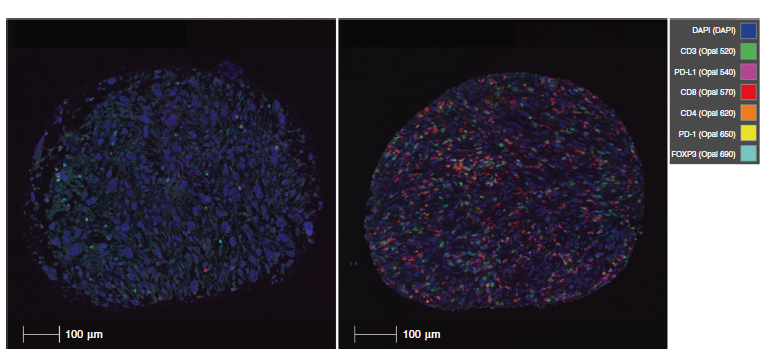
该回顾性研究共纳入了192名接受手术治疗的STS患者(中位年龄为63.5 岁,其中有103名男性(53.6%))。通过构建组织微阵列,对PD-1、PD-L1、FOXP3、CD3、CD4和CD8等标志物进行免疫组化分析。并分析TIL表型丰度和免疫检查点标记物与患者上述临床参数(LR、DM和OS)的相关性。
两种粘液纤维肉瘤的多光谱图像
研究人员发现,除FOXP3+和CD3-PD-L1+细胞亚群外,不同组织学亚型与所有免疫检查点标记物之间存在显著差异。相比于平滑肌肉瘤,粘液纤维肉瘤中发现了更高水平的PD-L1、PD-1和所有TIL表型。
进一步的研究发现,Tregs的存在与LR的风险升高相关,与手术切缘无关。其他TIL或免疫检查点标记物对患者的结果参数并无显著影响。
免疫检查点标记物和TIL表型的丰度取决于组织学亚型
总而言之,该研究结果发现,TIL和免疫检查点标记物在粘液纤维肉瘤中的水平最高。无论患者的手术切缘状态如何,高Treg水平均与患者的LR风险升高独立相关。
原始出处:
Smolle, M.A., Herbsthofer, L., Granegger, B. et al. T-regulatory cells predict clinical outcome in soft tissue sarcoma patients: a clinico-pathological study. Br J Cancer (14 June 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








.jpg)




#临床结果#
38
#软组织#
31
学习了
74
学习
64