Nature:胶质母细胞瘤进展,新途径可避开血脑屏障,显著延长生存期!
2020-01-19 Ruthy 转化医学网
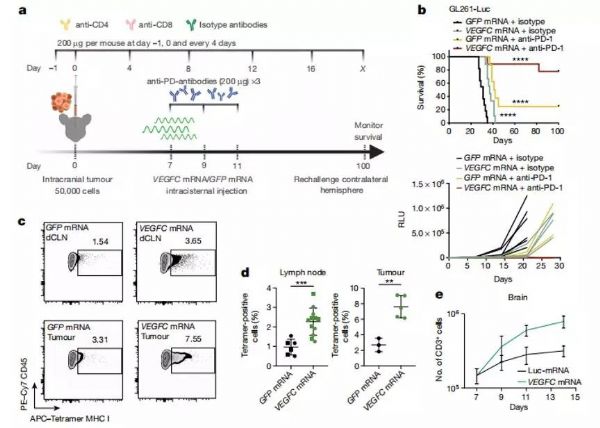
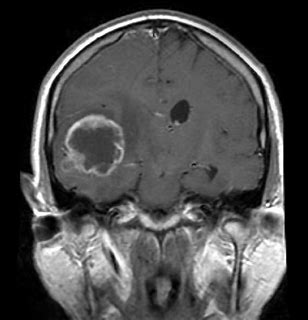
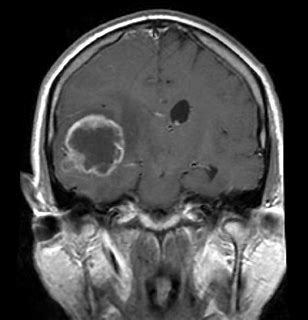
导 读:胶质母细胞瘤(GBM)是最为常见且难以治愈的原发性脑部肿瘤,患者术后预后普遍不佳,即使有放疗相助,患者5年生存率仍然低于10%。肿瘤免疫治疗的发展给多种不治之症的治疗带来了新希望,但大脑独特的免疫环境将大多数治疗药物拦截在外,导致该疗法在GBM治疗领域裹足不前。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#新途径#
37
#胶质母细胞#
27
#母细胞瘤#
37
#Nat#
32
#血脑屏障#
32
#生存期#
18
#细胞瘤#
23