JPD: 鉴别痴呆的脑脊液生物标记物,是否可用来鉴别帕金森病?
2022-05-23 Freeman MedSci原创
预测认知障碍的t-tau和p-tau的最佳临界值明显低于AD临界值,
至少有75%的帕金森病(PD)患者会长期发展为痴呆,极大地影响了他们的生活质量。轻度认知障碍(MCD)往往在PD患者痴呆之前出现,大约有25-30%的PD患者没有痴呆,但会出现MCI。
图1: 论文封面图
由于全世界有超过400万人受到PD的影响,目前还没有有效的治疗方法,建立生物标志物来识别早期和快速认知能力下降的高风险患者是研究和临床的关键。 通过使用生物标志物对不同的早期帕金森病患者进行分层,将有助于开发和实施针对特定帕金森病症状的临床试验,并且了解哪些患者可能会出现认知能力下降,使医生为向患者及其家属传达预后做好准备。
帕金森病认知障碍的基本病理通常是皮质路易体包涵体与α-突触核蛋白(SYN)共存,这是与阿尔茨海默病(AD)的淀粉样β(Aβ)斑块和tau神经纤维缠结相关性最强的病理措施。
大约三分之一的帕金森病痴呆患者同时存在AD病理,这与SYN病理增加有关,导致认知能力更快下降。 这些错误折叠的蛋白质,除了神经元结构和活动的变化外,被认为是导致认知障碍的原因,因为SYN、Aβ和tau的神经病理标志物的组合被认为与突触的丧失、神经递质的影响、线粒体功能障碍和神经炎症协同作用,影响PD的认知。 PD、PD与痴呆(PDD)、AD和路易体痴呆(DLB)的病理重叠,以及了解这与不同疾病的认知障碍之间的关系,是目前人们非常感兴趣的一个领域。
脑脊液(CSF)中预测进展为认知障碍的生物标志物已被广泛研究,其中一些发现在PD中得到支持。淀粉样β1-42(Aβ1-42)的水平下降,总tau(t-tau)的水平增加,以及磷酸化tau(p-tau)的水平增加,都可以预测这两种疾病的进展为认知障碍,其中Aβ1-42是PD中最强的预测因素。
一些研究表明,AD CSF生物标志物的病理水平在PD人群中具有较差的预后性(在AD队列中)。
藉此,宾夕法利亚大学大学的Sarah Weinshela等人, 使用两个指标(基线和纵向认知障碍,以及PET淀粉样蛋白成像)来研究这个问题。
他们首先调查了基于既定AD分界线的生物标志物的二元分类在预测PD的认知障碍时是否与连续生物标志物表现类似。 为了更直接地评估将AD的CSF生物标志物分界线应用于早期PD患者的适当性,
他们根据PPMI队列计算了生物标志物的最佳分界线,同时使用认知测试和在有淀粉样蛋白成像的患者子集中使用体内检测作为斑块病理学的代理。
然后,将这些最佳分界线的大小和预测能力与AD分界线进行了比较,目的是确定是否应该建立PD的具体分界线。
他们旨在评估已建立的源自AD的CSF生物标志物预测Aβ和tau病理的截止点的适用性和诊断准确性。
他们使用帕金森病进展标志物倡议(PPMI)队列中423名新诊断的PD患者的CSF生物标志物、认知诊断和PET淀粉样蛋白成像的基线和纵向数据,与来自PPMI队列的最佳截止值相比,评估既定的AD生物标志物截止值。
他们将PET淀粉样蛋白成像作为AD病理学的金标准,Aβ 142的最佳截止值高于AD截止值,t-tau/Aβ 142和p-tau/Aβ 142的最佳截止值低于AD截止值,而且它们的置信区间(CIs)与AD截止值不重合。
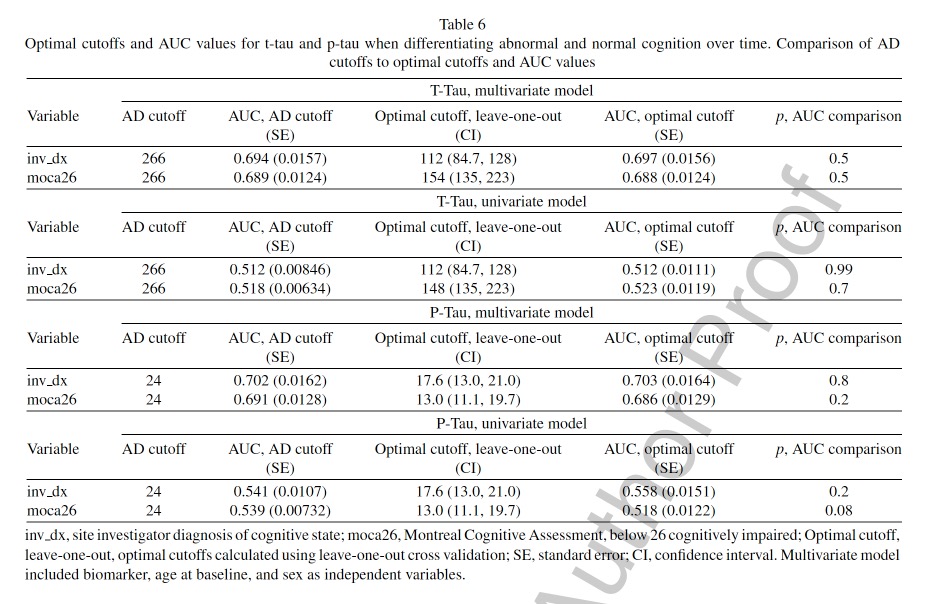
图2:论文结果图
预测认知障碍的t-tau和p-tau的最佳临界值明显低于AD临界值,而且它们的置信区间(CIs)与AD临界值不重叠。
PPMI队列中预测淀粉样蛋白-PET阳性的Aβ 1-42、t-tau/Aβ 1-42和p-tau/Aβ 1-42以及预测认知障碍的t-tau和p-tau的最佳分界线与来自AD人群的分界线有很大不同。
PD中存在额外的病理现象,如α-突触蛋白,可能导致疾病特定的CSF生物标志物特征。
原文出处:
Weinshel, S., Irwin, D. J., Zhang, P., Weintraub, D., Shaw, L. M., Siderowf, A., & Xie, S. X. (2022). Appropriateness of Applying Cerebrospinal Fluid Biomarker Cutoffs from Alzheimer’s Disease to Parkinson’s Disease. _Journal of Parkinson’s Disease_, 1–13. [https://doi.org/10.3233/JPD-212989](https://doi.org/10.3233/JPD-212989)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#标记物#
34
学习了,谢谢分享
33
#生物标记#
0
#生物标记物#
36
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
30