Radiology:基于ACR TI-RADS特征的甲状腺结节超声诊断的人工智能模型
2022-08-13 shaosai MedSci原创
深度学习是人工智能(AI)的一个子集,具有强大的自主特征提取和特征表达能力。
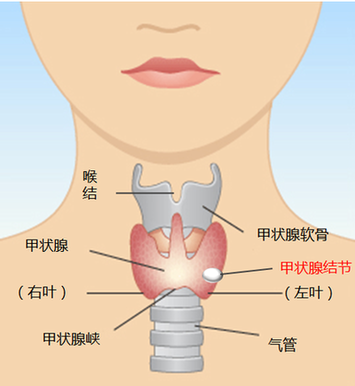
 甲状腺结节在临床实践中极为常见,有65%的甲状腺结节是通过超声检查被发现的,所有甲状腺结节中约有10%是恶性的。然而,结节的高检出率可能导致过度诊断和过度治疗。为了提高US的诊断准确性,美国放射学会在2017年发布了甲状腺成像报告和数据系统(TI-RADS),可以提高甲状腺结节分层的性能。
甲状腺结节在临床实践中极为常见,有65%的甲状腺结节是通过超声检查被发现的,所有甲状腺结节中约有10%是恶性的。然而,结节的高检出率可能导致过度诊断和过度治疗。为了提高US的诊断准确性,美国放射学会在2017年发布了甲状腺成像报告和数据系统(TI-RADS),可以提高甲状腺结节分层的性能。
深度学习是人工智能(AI)的一个子集,具有强大的自主特征提取和特征表达能力。一些研究报告称,与重要的US特征相结合的深度学习可以达到类似于或优于有经验的放射科医生的甲状腺结节的诊断性能。然而,并没有有研究将具有重要US特征的深度学习与没有US特征的深度学习和初级放射科医生进行比较。
近日,发表Radiology杂志的一项研究在多任务深度学习的基础上,利用TI-RADS特征(以下简称MTI-RADS)开发了用于甲状腺结节分类的人工智能模型。并与应用TI-RADS的放射科医生进行了比较,为临床更准确的进行甲状腺结节的风险分层提供了参考依据。
这项回顾性研究纳入了来自636名连续患者(平均年龄,49岁±14[SD];485名女性)的1588个经手术证实的甲状腺结节。对1345个结节的US图像进行了MTI-RADS和MDiag训练(2018年1月至2019年12月)。在测试数据集(243个结节,2019年1月至2019年12月)上,使用DeLong方法和McNemar检验比较了MTI-RADS和MDiag以及不同经验水平的放射科医生的性能。
MTI-RADS的AUC和敏感性分别为0.91和83%(66个结节中的55个),与有经验的放射医师(0.93[P=0.45]和92%[66个结节中的61个;P=0.07])没有明显差异,且超过了初级放射医师(0.78[P<0.001]和70%[66个结节中的46个;P=0.04])。MTI-RADS的特异性(87%[177个结节中的154个])高于有经验和初级放射医师的特异性(分别为80%[177个结节中的141个;P=.02]和75%[177个结节中的133个;P=.001])。MTI-RADS的AUC高于MDiag(分别为0.91 vs 0.84;P = .001)。在243个结节的测试组中,MTI-RADS和有经验组的一致性率高于MTI-RADS和初级组的一致性率(分别为79% [n = 193] vs 73% [n = 178];P = . 02)、回声率(75% [n = 183] vs 68% [n = 166]; P = .04)、形状(93% [n = 227] vs 88% [n = 215]; P = .04)以及边缘光滑或不清晰(72% [n = 174] vs 63% [n = 152]; P = .002)。
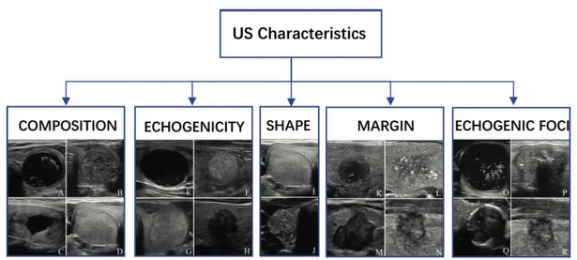
图 具有五个美国放射学会甲状腺成像报告和数据系统特征的US图像示例。构成特征包括(A)囊性或几乎完全囊性、(B)海绵状、(C)囊性和实性混合以及(D)实性或几乎完全实性。回声特征包括(E)无回声、(F)高回声、(G)等回声,和(H)低回声。形状特征包括(I)宽于高,(J)高于宽。边缘特征包括(K)光滑、(L)不明确、(M)分叶状或不规则、(N)甲状腺外扩展。回声灶特征包括(O)无或大彗尾伪影,(P)大钙化、(Q)周边钙化、和(R)点状回声灶
本研究表明,基于美国放射学会甲状腺成像报告和数据系统特征的人工智能模型在甲状腺结节的诊断中具有良好的诊断性能。
原文出处:
Yufan Chen,Zixiong Gao,Yanni He,et al.An Artificial Intelligence Model Based on ACR TI-RADS Characteristics for US Diagnosis of Thyroid Nodules.DOI:10.1148/radiol.211455
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TI-RADS#
49
#ADS#
58
#RADS#
41
#ACR#
41
#超声诊断#
35
#超声诊断#
41